You are here: Urology Textbook > Kidneys > Acute pyelonephritis > Definition and epidemiology
Acute Pyelonephritis: Definition and Causes
- Acute pyelonephritis: definition, causes, and pathology
- Acute pyelonephritis: symptoms and diagnostic workup
- Acute pyelonephritis: treatment
Guidelines: EAU Guidelines Urological Infections, (German S3 Guidelines UTI).
Definition of Acute Pyelonephritis
Acute pyelonephritis is a bacterial infection of the renal pelvis and the renal parenchyma with fever, flank pain, and bacteriuria. Standard laboratory tests cannot prove bacterial infection of the kidney; acute pyelonephritis is defined clinically as a urinary tract infection with flank pain, flank tenderness, or fever.
Uncomplicated pyelonephritis:
Acute pyelonephritis limited to non-pregnant women before menopause, without anatomical or functional abnormalities of the urinary tract, or infection-promoting comorbidities.
Complicated pyelonephritis:
All patients with pyelonephritis, which is not classified as uncomplicated: in males or pregnant women, patients with anatomical deformities, bladder catheter, renal disease or infection-promoting comorbidities.
Etiology (Causes) of Pyelonephritis
Ascending Infection:
Ascending infection is the most common cause of acute pyelonephritis. Since the female urethra is short and intestinal bacteria tend to colonize the perineum and vulva, women have significantly more often bladder infections and pyelonephritis than men. See section Causes of urinary tract infections.
Vesicoureteral Reflux:
Vesicourethral reflux (VUR) leads to refluxing urine, which becomes infected. Pyelonephritis in VUR tends to cause renal scarring, since intrarenal reflux is common. The anatomy of the papillae causes intrarenal reflux, especially at the renal poles. See also the section "Vesicoureteral reflux".
Renal Scarring due to Pyelonephritis:
Recurrent relapses of acute pyelonephritis produce renal scarring in children. Chronic pyelonephritis and Ask-Upmark kidney may develop. New renal scarring is uncommon beyond five years but may occur until puberty.
The cause for the vulnerability of the child's kidney to renal scarring is explained with the following mechanisms:
- intra-renal reflux happens with much lower vesical pressures than in adulthood
- decreased immunocompetence for bacterial infections in the first years of life
- clinical difficulties in the early diagnosis of pyelonephritis in the first years of life
Pyelonephritis in Pregnancy:
The incidence of bacteriuria in pregnancy is 4–7%, comparable to the rate of bacteriuria without pregnancy. Of these patients with bacteriuria, approximately 20–30% develop acute pyelonephritis (1–4% of all pregnant women). The most common manifestation of pyelonephritis is the second trimester.
Complications of pyelonephritis during pregnancy: anemia (23%), sepsis (17%), transient renal failure (2%), pulmonary complications (7%), and premature births (rare). See section urinary tract infections in pregnancy.
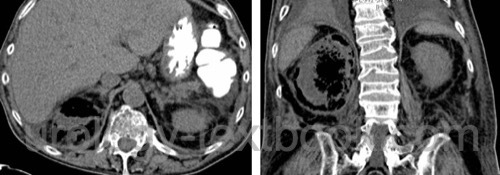
Emphysematous Pyelonephritis:
Emphysematous pyelonephritis is a serious complication of acute pyelonephritis with high mortality (43%). Risk factors for emphysematous pyelonephritis are diabetes mellitus or upper urinary tract obstruction. Most probably, E. coli causes gas formation by fermentation. The gas remains restricted within the renal fascia.
Emphysematous pyelonephritis must be distinguished from a renal abscess, which may also contain gas. The renal abscess has a favorable prognosis after drainage and antibiotic treatment.
 |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
Common Pathogens of Acute Pyeloneprhitis
Gram-negative pathogens
E. coli, Klebsiella, Enterobacter, Serratia, Pseudomonas, Proteus mirabilis, and other gram-negative coliform bacteria in 80%.
Gram-positive pathogens
Staphylococcus aureus, Staph. saprophyticus, Enterococci.
Fungi
Candida (rare).
Pathologic Findings
Gross Pathology
- Enlarged kidney with inflammatory edema
- Small subcapsular abscesses with hemorrhagic rim
- Pus-filled tubules
- The urothelium of the renal pelvis is thick and covered with exudate
Histology of Acute Pyelonephritis
Microscopy shows dense granulocytic inflammation and tissue destruction with liquefaction in the renal parenchyma and renal pelvis. The inflammation affects mainly the tubules, and the glomeruli are less affected.
| Kidney diseases | Index | Symptoms PN |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
G. Bonkat, R. Bartoletti, F. Bruyère, S. E. Geerlings, F. Wagenlehner, and B. Wullt, “EAU Guideline: Urological Infections.” [Online]. Available: https://uroweb.org/guidelines/urological-infections/
DGU, DEGAM, and PEG, “S3 Leitlinie Epidemiologie, Diagnostik, Therapie, Prävention und Management unkomplizierter, bakterieller, ambulant erworbener Harnwegsinfektionen bei erwachsenen Patienten Aktualisierung 2024.” [Online]. Available: https://register.awmf.org/assets/guidelines/043-044l_S3_Epidemiologie-Diagnostik-Therapie-Praevention-Management-Harnwegsinfektione-Erwachsene-HWI_2024-09.pdf
Dalla-Palma und Pozzi-Mucelli 2000 DALLA-PALMA, L. ;
POZZI-MUCELLI, F.:
[The imaging of chronic renal infections].
In: Radiologe
40 (2000), Nr. 6, S. 537–46
Fihn 2003 FIHN, S. D.:
Clinical practice. Acute uncomplicated urinary tract infection in
women.
In: N Engl J Med
349 (2003), Nr. 3, S. 259–66
Kawashima u.a. 2000 KAWASHIMA, A. ; SANDLER,
C. M. ; GOLDMAN, S. M.:
Imaging in acute renal infection.
In: BJU Int
86 Suppl 1 (2000), S. 70–9
Nickel 2001 NICKEL, J. C.:
The management of acute pyelonephritis in adults.
In: Can J Urol
8 Suppl 1 (2001), S. 29–38
Roberts 1999 ROBERTS, J. A.:
Management of pyelonephritis and upper urinary tract infections.
In: Urol Clin North Am
26 (1999), Nr. 4, S. 753–63
 Deutsche Version: Akute Pyelonephritis
Deutsche Version: Akute Pyelonephritis
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as a Kindle e-book on Amazon—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students.