You are here: Urology Textbook > Anatomy > Urinary bladder
Histology and Layers of the Urinary Bladder Wall
References: (Benninghoff, 1993).
Urothelium (Transitional Epithelium): Mucosa of the Bladder
The mucosa of the urinary bladder is lined by a multilayered transitional epithelium (urothelium). The mucosa with a special GAG layer enables the storage of urine with high osmolarity.
Histology of the Transitional Epithelium:
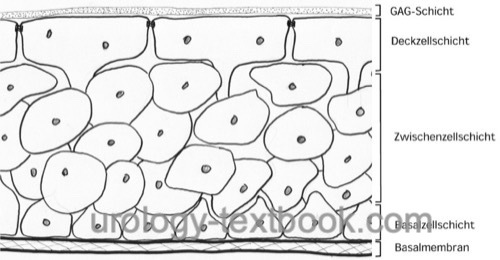
Urothelium is a multilayered epithelium with a maximum of seven cell layers [fig urothelium]. There are three different cell types: basal cell layer, intermediate cell layer, and surface cell layer. The basal cell layer renews the urothelium by cell division. The new cells migrate to the lumen. The surface cells are large epithelial cells, sometimes multinucleate, up to 200 μm in size. The enormous elasticity of the urothelium, and in particular of the surface cells, is explained with subapical vesicles. With increasing bladder stretch, the subapical vesicles are built into the cell membrane (exocytosis).
 |
Squamous metaplasia of the bladder trigone:
Squamous metaplasia of the bladder trigone occurs in 30–70% of women and much less frequently in men. On cystoscopy, squamous metaplasia appears as a dull mucosa with a coating and is usually sharply limited to the trigonum of the urinary bladder. Synonyms: trigonal leukoplakia, pseudomembranous trigonitis. According to current knowledge, typical squamous metaplasia in the trigonum has no pathological value and must be differentiated from atypical metaplasia of the urinary bladder due to chronic inflammation.
GAG layer of the bladder:
The surface cells are covered by a glycosaminoglycan layer (GAG). The function of the GAG layer is controversial; suggested tasks are an osmotic barrier function and an antibacterial coating of the urothelium (low adherence of the bacteria).
Osmotic gradient:
There is a high osmotic and chemical gradient between the urine and the blood plasma. The following mechanisms of the urothelium protect the passage of urine into the lamina muscularis: GAG-layer, surface cells (4 to 6 tight junctions), uroplakin proteins in the apical cell membrane, and a capillary plexus in the submucosa.
Despite the factors mentioned above, substances permeate from the urine into the plasma. This is most evident for water and urea. Passive diffusion and active transport change metabolite concentrations in the urine while in the urinary bladder over time.
Submucosa (Lamina Propria) of the Bladder Wall
The submucosa of the transitional epithelium consists of connective tissue (collagen, elastin, and other extracellular matrix proteins). Beneath the urothelium, there is a dense capillary plexus. In addition to the vascular supply of the urothelium, the capillary plexus serves as a barrier function. Substances that penetrate through the urothelium are removed, and the muscular layer of the bladder wall is protected against urine. Due to the strong elasticity of the vascular plexus, a regular filling of the bladder does not increase the vascular resistance of the submucosal plexus. In contrast to excessive filling, vascular resistance will rise together with increasing bladder wall tension.
Tunica muscularis of the bladder
The tunica muscularis of the bladder is formed by the detrusor muscle, which consists of smooth muscle cells. The muscle fibers run irregularly in all directions. Only at the bladder trigone, the detrusor muscle consists of three layers (see trigone of the urinary bladder).
Histology of the smooth muscle layer:
The tunica muscularis contains spindle-shaped muscle cells, which are connected to each other. The cells contain actin and myosin as contractile elements, but they are disorganized and do not form sarcomeres. The myofibrils move across the smooth muscle cell from cell wall to cell wall, producing a shortening and thickening of the muscle cell with contraction. In the relaxed state, smooth muscle cells are several hundred μm long and 5–6 μm thick.
Extracellular matrix of the tunica muscularis:
An elastic connective tissue stroma of collagen (e.g., I, III, IV) and elastin stabilizes the bladder wall. The ratios of connective tissue proteins to each other and the relationship of smooth muscle cells to the extracellular matrix are essential for the elasticity (compliance) of the bladder.
| Bladder, Anatomy | Index | Bladder, Function |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Benninghoff 1993 BENNINGHOFF, A.:
Makroskopische Anatomie, Embryologie und Histologie des
Menschen.
15. Auflage.
München; Wien; Baltimore : Urban und Schwarzenberg, 1993
 Deutsche Version: Histologie der Harnblase
Deutsche Version: Histologie der Harnblase
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.