You are here: Urology Textbook > Surgery (procedures) > Cystoscopy
Cystoscopy: Indications, Technique (Step by Step) and Complications
Cystoscopy is the endoscopic examination of the urethra and urinary bladder with a cystoscope. It is recommended in the following situations:
- Microhematuria and hematuria
- LUTS
- Recurrent urinary tract infections
- Suspected urethral or bladder diseases (fistula, foreign body, diverticula)
- Suspected bladder tumor
- Follow-up examinations after carcinoma of the urethra or bladder
Contraindications of Cystoscopy
Relative Contraindication: urinary tract infections.
Equipment for Cystoscopy
Rigid Cystoscope:
The rigid cystoscope consists of a sheath (17–22 CH), an obturator, and an optical lens. The bridge connects the lens to the sheath and allows a working channel to insert forceps, wires or ureteral stents [fig. rigid cystoscope]. The obturator blunts the sheath for blind passage into the bladder. Optical lenses are available with different tip angles: 0° for endoscopy of the urethra and 30° or 70° for endoscopy of the bladder.
 |
Flexible Cystoscope:
The diameter is between 16–20 CH, and the distal end of the cystoscope is actively steerable [fig. flexible cystoscope]. The working channel (up to 8 CH) allows the insertion of forceps or ureteral stents. Modern devices do not use fiber optics; a camera chip (CCD sensor) on the tip provides a high-resolution image of high quality.
 |
The Technique of Cystoscopy: Step by Step
Patient Preparation:
Lithotomy positioning for rigid cystoscopy, supine positioning or lithotomy positioning for flexible cystoscopy. Local anesthesia of the urethra with anesthetic lubricant is usually sufficient; in children and anxious patients, sedation or anesthesia is necessary. Antibiotic prophylaxis is unnecessary if the urine is sterile.
Rigid Cystoscopy:
The cystoscope is inserted in women blindly, the obturator is used to blunt the sheath for a safe blind passage. In men, the cystoscope is advanced into the urinary bladder under vision, and the urethra and prostate are examined at the same time with a 0° optical lens. The bladder is better examined with a 30° or 70° optical lens. While every part of the bladder is systematically examined (trigonum, orifices, posterior wall, lateral walls, and anterior wall), overdistension of the urinary bladder with the irrigation fluid must be avoided.
Flexible cystoscopy:
Flexible cystoscopy offers significant advantages (less pain) for examining men. An assistant or the fourth and fifth fingers of the left hand stretch the penis and urethra, and the remaining fingers of the left hand move the cystoscope shaft forward or backward. The right hand guides the cystoscope with a fist grip on the handpiece, the thumb of the right hand controls the flexion of the distal tip [fig. flexible cystoscope]. With maximum irrigation, the urethra and prostate are examined first, followed by the trigonum, orifices, posterior wall, lateral walls, and anterior wall of the bladder using a standardized scheme.
Fluorescence Cystoscopy:
Fluorescence cystoscopy with blue light after prior instillation of hexaminolevulinate (Hexvix) leads to better detection of urinary bladder carcinoma, especially flat lesions such as CIS (Jocham et al., 2005). See section turb for further details.
Normal Findings and Procedure Report
Female Urethra:
The passage of the sheath is possible without resistance, the urethral mucosa presents without exophytic lesions of inflammation.
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
Male Urethra:
The scope passes easily through the urethra, there are no exophytic tumors, inflammation, or narrowing of the urethral mucosa. The sphincter contracts when the irrigation is stopped.
 |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
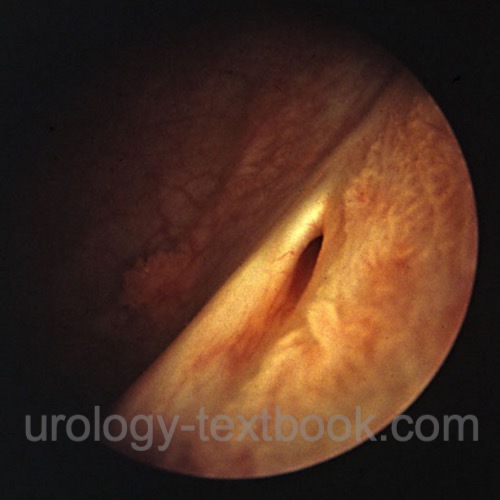
Prostate:
The normal length of the prostatic urethra is below 3 cm (from the seminal colliculus to the bladder neck). Note signs of bladder neck obstruction like enlarged prostatic lobes, presence of a median lobe or an elevated bladder neck. Rule out exophytic or inflammatory lesions of the prostatic urethra.
 |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
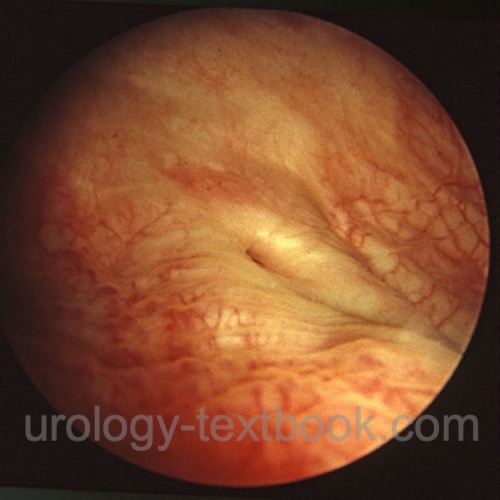
Bladder:
The urethral orifices are orthotopic and slit-shaped, with no signs of reflux. The outflowing urine is clear on both sides. The bladder mucosa is smooth (without trabeculation), shows a normal vascular pattern, no signs of inflammation or exophytic masses. The frequently occurring squamous metaplasia of the trigonum in women is seen on cystoscopy as a dull mucosa with a coating and is usually sharply limited to the trigonum of the urinary bladder.
 |
 |
 |
Complications of Cystoscopy
- Pain
- Hematuria, usually harmless and self-limiting
- Urinary tract infection, the risk of febrile UTI is 1% in patients with sterile urine (Herr, 2014)
- Significant injury to the urethra, prostate, and bladder is rare
- Urinary retention is possible after cystoscopy in men with BPH
| Urologic Surgery | Index | TURB |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Burke DM, Shackley DC, O'Reilly PH. The community-based morbidity of flexible cystoscopy. BJU Int. 2002 Mar;89(4):347-9. doi: 10.1046/j.1464-4096.2001.01899.x.
Herr HW. Should antibiotics be given prior to outpatient cystoscopy? A plea to urologists to practice antibiotic stewardship. Eur Urol. 2014 Apr;65(4):839-42. doi: 10.1016/j.eururo.2013.08.054.
 Deutsche Version: Zystoskopie
Deutsche Version: Zystoskopie
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.