You are here: Urology Textbook > Testes > Fournier gangrene
Fournier Gangrene: Treatment of Perigenital Necrotizing Fasciitis
Definition of Fournier Gangrene
Fournier gangrene is a form of necrotizing fasciitis of the genital and perineal region.
 |
Epidemiology
The incidence in the USA is 1.6/100,000 and mainly affects men over 50 years of age
.Etiology (Causes) of Fournier Gangrene
Bacteriology:
The origin of the mixed infection with aerobe and anaerobe bacteria is the skin, the urinary tract, or the rectum. There is probably a synergy between anaerobic (Bacteroides, Fusobacterium, Clostridium ...) and aerobic bacteria (E. coli, Enterococci, Klebsiella ...).
Risk factors:
- Diabetes mellitus
- Trauma or surgery of the perigenital region
- Urethral extravasation of urine
- Urethral injury
- Paraphimosis
- Rectal injury
Pathophysiology:
The Fournier gangrene spreads along the superficial perigenital fascial planes, leading to local vascular thrombosis, ischemia, and necrosis. Deeper infections with myonecrosis are not typical. The ischemia in the tissue enables the growth of anaerobic bacteria.
Signs and Symptoms of Fournier Gangrene
- Local swelling, redness, tumor, crepitus (gas formation).
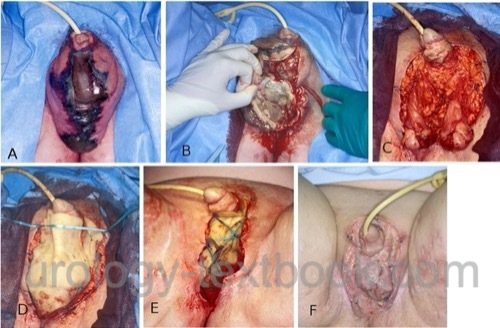
- In progredient disease, dark hemorrhagic necrotic areas develop [fig. Fournier gangrene of the scrotum].
- Fast spreading of the necrosis (up to 2~cm per hour)
- Fever, signs of sepsis
Diagnostic Workup in Fournier Gangrene
Blood tests:
- Differential blood count, coagulation tests, CRP, electrolytes, liver values, creatinine, urea, blood gas analysis and procalcitonin.
- Microbiology: wound swab culture, urine culture and blood culture
Ultrasound Imaging of the Scrotum:
Signs of testicular infection? Epididymitis? Trapped air in scrotal tissue?
CT Abdomen/Pelvis
CT is indicated if a colorectal origin of the Fournier gangrene is suspected. Trapped air in the tissue indicates the extent of the Fournier gangrene.
Treatment of Fournier Gangrene
Fournier gangrene is a urologic emergency. Timely diagnosis with immediate initiation of antibiotics, early management of sepsis, and prompt radical excision of the necrosis can significantly improve the prognosis.
Antibiotic therapy:
Antibiosis must cover a broad spectrum of gram-negative, gram-positive, aerobic, and anaerobic bacteria. Due to the severe infection, antibiotics are prescribed in the highest possible dosage. The calculated initial antibiotic therapy must be adjusted after receiving the antibiogram and resistance testing. The following options are useful:
- Carbapenems (imipenem, meropenem or ertapenem).
- Piperacillin/tazobactam and vancomycin
- Cephalosporin (third generation) and metronidazole
- Aminopenicillin, gentamicin and metronidazole
Surgical Debridement:
Surgical debridement includes wound swabs and radical resection of gangrenous tissue until healthy tissue is reached [fig. Surgical treatment of Fournier gangrene]. Orchiectomy is rarely necessary. For open wound healing, the testicles can be secured in subcutaneous thigh pockets. After 24–48 h, a second look operation with surgical debridement is necessary to ensure complete removal of necrotic tissue. Secondary wound closure is sometimes possible to speed up wound healing.
Suprapubic catheter:
If catheter drainage is necessary, a suprapubic catheter should be preferred.
Colostomy:
If the origin of Fournier gangrene is the rectum, a colostomy is mandatory. A colostomy is also sometimes necessary in cases of extensive perineal gangrene for wound care reasons.
Surgical Reconstruction:
Surgical reconstruction of large defects is done with skin grafts or flaps.
Prognosis of Fournier Gangrene
Mortality of Fournier gangrene is around 20%. Risk factors of increased mortality are diabetes mellitus, alcoholism and colorectal origin of Fournier gangrene (often delayed diagnosis and extensive infection).
| Mumps orchitis | Index | Testicular torsion |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
G. Bonkat, R. Bartoletti, F. Bruyère, S. E. Geerlings, F. Wagenlehner, and B. Wullt, “EAU Guideline: Urological Infections.” [Online]. Available: https://uroweb.org/guidelines/urological-infections/
Montrief T, Long B, Koyfman A, Auerbach J. Fournier Gangrene: A Review for Emergency Clinicians. J Emerg Med. 2019 Oct;57(4):488-500. doi: 10.1016/j.jemermed.2019.06.023.
Nomikos 1998 NOMIKOS, I. N.:
Necrotizing perineal infections (Fournier’s disease): old remedies
for an old disease.
In: Int J Colorectal Dis
13 (1998), Nr. 1, S. 48–51
Papachristodoulou u.a. 1997 PAPACHRISTODOULOU, A. J. ;
ZOGRAFOS, G. N. ; PAPASTRATIS, G. ; PAPAVASSILIOU,
V. ; MARKOPOULOS, C. J. ; MANDREKAS, D. ; GOGAS,
J. G.:
Fournier’s gangrene: still highly lethal.
In: Langenbecks Arch Chir
382 (1997), Nr. 1, S. 15–8
 Deutsche Version: Fournier-Gangrän
Deutsche Version: Fournier-Gangrän