You are here: Urology Textbook > Testes > Hydrocele
Hydrocele testis: Causes, Diagnosis and Treatment
Definition and Classification of Hydroceles
Hydrocele testis
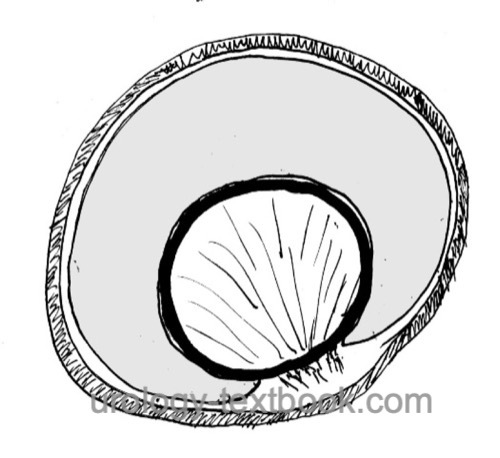
A hydrocele testis is an accumulation of serous fluid in the cavity of the tunica vaginalis of the testis, without communication of the hydrocele with the abdominal cavity [hydrocele testis].
Funiculocele or Hydrocele of the Spermatic Cord
A funiculocele or hydrocele of the spermatic cord is an accumulation of serous fluid in a non-obliterated part of the processus vaginalis without communication with the abdominal cavity or tunica vaginalis of the testis.
Communicating Hydrocele
An open processus vaginalis leads to varying amounts of serous fluid in the cavum vaginalis testis.
Abdominoscrotal Hydrocele
The inguinal portion of a large hydrocele extends into the low pressure compartment of the abdomen. An obliteration of the hydrocele develops in the area of the internal inguinal ring.
 |
Etiology of Hydroceles
Congenital Hydroceles
With the descent of the testis, the parietal peritoneum forms the processus vaginalis and the cavity of the tunica vaginalis of the testis. The processus vaginalis usually obliterates till the fourth month of life. The failure of processus vaginalis closure leads to congenital communicating hydroceles.
Acquired Hydroceles
There is a balance between fluid production and outflow in the cavity of the tunica vaginalis. The following diseases disturb the balance: inflammation, tumors, testicular trauma, torsion of the testis or testicular appendages, and impaired lymphatic drainage (after surgery for varicoceles or inguinal hernias).
Signs and Symptoms
- Painless scrotal swelling, positive transillumination
- Communicating hydrocele: size is changing depending on activity (small in the morning, large in the evening).
Diagnosis of Hydrocele
Ultrasound Imaging
The typical testicular ultrasound imaging finding is an anechoic fluid collection in the cavity of the tunica vaginalis of the testis [fig. ultrasound of a hydrocele]. It is important to carefully examine the testes and spermatic cord (Testicular torsion? Tumor? Size of the epididymis? Septations? Abdominal parts of the hydrocele?).
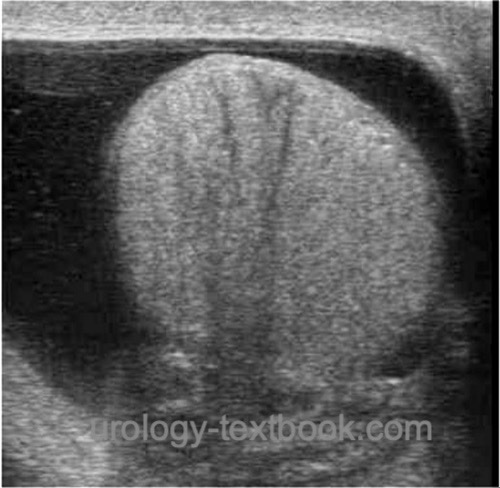 |
| Ultrasound imaging: hydrocele of the testis |
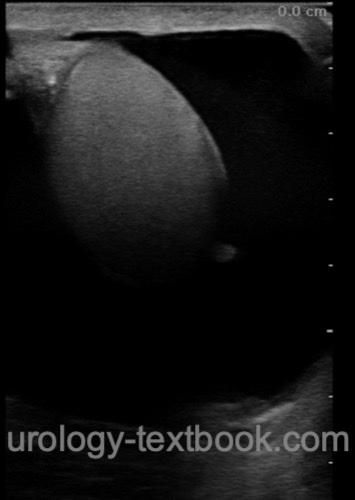 |
| Ultrasound imaging: hydrocele of the testis |
Differential Diagnosis of a Scrotal Swelling
The most important reasons for a painless scrotal swelling are:
- Hydrocele
- Spermatocele
- Varicocele
- Hematocele
- Scrotal hernia
- Testicular cancer
Treatment of Hydroceles
Please see the section hydrocelectomy: surgical techniques and complications for details.
Surgery for Communicating Hydroceles
Treatment of communicating hydroceles starts with an inguinal incision for exposure of the testis. The processus vaginalis is isolated from the spermatic cord, divided, and ligated at the internal inguinal ring. The distal sac is resected as far as possible, and the end of the sac can be left open.
Contralateral exploration is not a standard therapy, but is sometimes performed. The probability for an open contralateral processus vaginalis in unilateral communicating hydrocele is 50%, but only about 15–22% become clinically significant.
Surgery for Hydroceles of the Cord
Choose an inguinal incision for the approach to the spermatic cord. Mobilize and excise the hydrocele and ligate the processus vaginalis at the internal inguinal ring.
Surgery for Hydroceles of the Testis
After a scrotal incision for exposure of the hydrocele, two surgical techniques are possible. The recurrence rate should be below 5% with either method; the Lord technique probably has the lowest complication rate:
- Hydrocelectomy with excision of the hydrocele sac: Winkelmann's technique or Jaboulay's technique
- Hydrocelectomy with plication of the hydrocele sac: Lord technique
Sclerotherapy for Testicular Hydroceles
Sclerotherapy is a therapeutic alternative to surgery for simple hydroceles of the testis and patients unfit for surgery. The recurrence rate is higher than with surgical therapy. After treatment failure of sclerotherapy, the surgical treatment is more difficult due to scarring and adhesions. Phenol 2.5% is used as a sclerosant.
| Varicocele | Index | Spermatocele |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Ku u.a. 2001 KU, J. H. ; KIM, M. E. ;
LEE, N. K. ; PARK, Y. H.:
The excisional, plication and internal drainage techniques: a
comparison of the results for idiopathic hydrocele.
In: BJU Int
87 (2001), Nr. 1, S. 82–4
Rubenstein u.a. 2004 RUBENSTEIN, R. A. ;
DOGRA, V. S. ; SEFTEL, A. D. ; RESNICK, M. I.:
Benign intrascrotal lesions.
In: J Urol
171 (2004), Nr. 5, S. 1765–72
C. Radmayr, G. Bogaert, H. S. Dogan, and S. Tekgül, “EAU Guidelines: Paediatric Urology.” [Online]. Available: https://uroweb.org/guidelines/paediatric-urology/
 Deutsche Version: Hydrozele: Ursachen und Therapie
Deutsche Version: Hydrozele: Ursachen und Therapie