You are here: Urology Textbook > Urologic surgery > Inguinal lymphadenectomy
Inguinal Lymphadenectomy: Technique of Groin Lymph Node Dissection
Indications for Inguinal Lymphadenectomy in Penile Cancer
Complete surgical removal of the inguinal and iliac lymph nodes offers the only chance of a cure for lymph node metastases of penile cancer. Since imaging cannot reliably detect lymph node metastasis, invasive lymph node sampling is recommended for patients with elevated risk for occult metastases: patients with pT1G2–3 and pT2–4 penile carcinoma. For a detailed discussion of the indication, see the section penile cancer.
 |
Contraindications
Bleeding disorders. Consider neoadjuvant chemotherapy and radiotherapy for patients with fixed lymph node metastases (cN3) with questionable resectability. The other contraindications depend on the surgical risk due to the patient's comorbidity and the surgical procedure's impact on the patient's life expectancy.
Surgical Technique of Inguinal Lymphadenectomy
Preoperative patient preparation:
- Perioperative antibiotic prophylaxis.
- Supine position with slight abduction in the hip and flexion in the knee.
- General anesthesia.
Surgical approach:
Skin incision 3 cm below and parallel to the inguinal ligament for inguinal lymphadenectomy. Bilateral iliac lymphadenectomy is possible via an extraperitoneal lower midline incision.
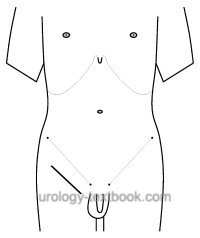 |
Superficial (modified) inguinal lymphadenectomy:
The modified inguinal lymphadenectomy (Catalona et al., 1988) reduces the dissection to the area above the fascia lata medial to the superficial epigastric vein and the great saphenous vein, which is also spared, see figure dissection areas for inguinal lymphadenectomy. Deep lymph nodes from the fossa ovalis are also removed. Lymph nodes may be sent to frozen section examination; alternatively, the final findings are awaited. If lymph node metastases are found, radical inguinal lymphadenectomy of the affected side is necessary.
Sentinel lymph node biopsy:
An alternative to superficial modified lymphadenectomy is the intraoperative detection and resection of the sentinel lymph node with the help of a gamma probe. Injection of a radioactive marker around the tumor is performed before surgery; in addition, injection of blue dye may facilitate intraoperative identification. Lymph nodes may be sent to frozen section examination; alternatively, the final findings are awaited.
Sentinel lymph node biopsy lowers the complication rate compared to superficial (modified) inguinal lymphadenectomy. The false-negative detection rate is 3–22% depending on the publication. If lymph node metastases are detected, ipsilateral radical inguinal lymphadenectomy is necessary. Contralaterally, a modified inguinal lymphadenectomy should be performed if sentinel lymph nodes are not detectable.
Radical ilioinguinal lymphadenectomy:
Radical inguinal lymph node dissection is necessary if lymph node metastases are detected in the abovementioned procedures. If two or more inguinal lymph node metastases are found or if lymph node metastases show extracapsular growth, ipsilateral radical iliac lymph node dissection is necessary for complete staging. In addition, radical inguinal lymphadenectomy is needed in patients with tumor recurrence in the groin during follow-up.
Inguinal radical lymphadenectomy:
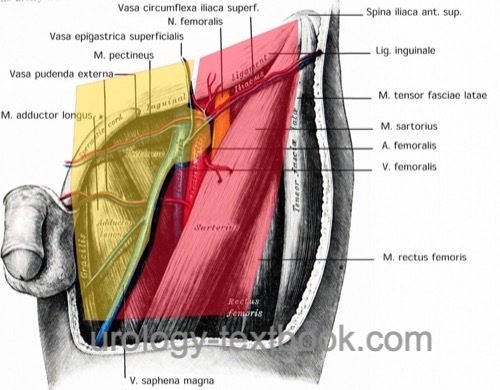
The dissection field is shown in fig. inguinal lymphadenectomy dissection fields. A careful dissection technique with bipolar coagulation, application of clips, or thin ligatures lowers the complication rate due to lymphoceles. Myocutaneous flaps are necessary to cover skin defects caused by large lymph node metastases. Incisional negative pressure wound therapy (iNPWT) lowers the rate of lymphoceles and wound healing complications.
Iliacal Lymphadenectomy:
Iliacal lymphadenectomy is done via an extraperitoneal lower midline incision. Dissection borders are laterally the external iliac artery, caudally the superior ramus of the os pubis, medially the obliterated umbilical artery and the urinary bladder, dorsally the obturator nerve and the pelvic wall, cranially the ureter and the bifurcation of the common iliac artery.
Postoperative Care
General measures:
Early mobilization, compression stockings, analgetics, thrombosis prophylaxis, heparin injections above the umbilicus, laboratory tests (hemoglobin, creatinine), and regular physical examination of the incision wound.
Drains:
Change dressings of the negative pressure wound therapy every 3 days, and keep the drains until drainage is below 30 ml/24 h.
Complications
Lymphedema, seroma, surgical site infections up to 40%, lymphocele, flap necrosis, venous thrombosis, pulmonary embolism. The number of removed lymph nodes, lymph node metastases, and the need for a large dissection field area are significant risk factors for complications.
| Radical penectomy | Index | Orchidopexy |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Cabanas 1977 CABANAS, R. M.:
An approach for the treatment of penile carcinoma.
In: Cancer
39 (1977), Nr. 2, S. 456–66
Catalona 1988 CATALONA, W. J.:
Modified inguinal lymphadenectomy for carcinoma of the penis with
preservation of saphenous veins: technique and preliminary results.
In: J Urol
140 (1988), Nr. 2, S. 306–10
Horenblas 2001 HORENBLAS, S.:
Lymphadenectomy for squamous cell carcinoma of the penis. Part 2: the
role and technique of lymph node dissection.
In: BJU Int
88 (2001), Nr. 5, S. 473–83
J. A. Smith, S. S. Howards, G. M. Preminger, and R. R. Dmochowski, Hinman’s Atlas of Urologic Surgery Revised Reprint. Elsevier, 2019.
 Deutsche Version: Technik und Komplikationen der inguinale Lymphadenektomie
Deutsche Version: Technik und Komplikationen der inguinale Lymphadenektomie