You are here: Urology Textbook > Surgery (procedures) > Laparoscopic nephrectomy
Surgical Steps and Complications of Laparoscopic Nephrectomy
Laparoscopic nephrectomy has clear advantages over open nephrectomy (less bleeding, postoperative pain, paralytic ileus, wound infection, and incisional hernia) and leads to a faster postoperative recovery of the patient.
Indications for Laparoscopic Nephrectomy
Benign diseases:
Nonfunctioning kidney with symptoms (e.g., bleeding, recurrent infections, nephrolithiasis, hydronephrosis, flank pain or renal hypertension).
Malignant diseases:
Renal cell carcinoma (up to 8 cm in size, depending on location) if partial nephrectomy is not feasible.
Contraindications for Laparoscopic Nephrectomy
Coagulation disorders. Do not perform radical nephrectomy if partial nephrectomy is technically possible, especially in patients with single kidneys, chronic kidney disease, bilateral renal cell cancer, or hereditary renal cell cancer. Choose the open surgical technique for large tumors (size >8 cm depending on location), lymph node metastasis, or vein thrombus. Consider the retroperiteoscopic or open surgical approach after major abdominal surgery (e.g., hemicolectomy of the same side). The other contraindications depend on the surgical risk due to the patient's comorbidity, the renal function of the contralateral kidney, and the surgical procedure's impact on the patient's life expectancy.
Surgical Technique of Laparoscopic Nephrectomy
Preoperative Preparations:
- Recommend a low fiber diet two days before surgery and a clear liquid diet on the preoperative day to improve the intraabdominal space.
- Administer an enema the night before surgery.
- Perioperative placement of a urinary catheter and gastric tube.
- Perioperative antibiotic prophylaxis is needed if risk factors for surgical site infections are present or if the urinary tract is planned to be opened.
- Insert a transurethral catheter and gastric feeding tube during surgery.
Surgical Approach Via Laparoscopy
Patient Positioning:
The patient is positioned in a lateral decubitus position at an angle of 45 degrees and with mild lumbar hyperextension. A vacuum mattress enables a secure fixation of the patient, even if the operation table has to be tilted.
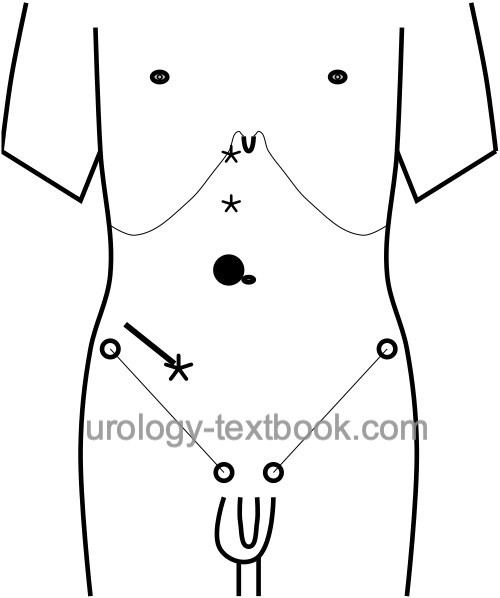
Trocar positions:
Create a Pneumoperitoneum with a mini-laparotomy or with the Veress needle next to the umbilicus (camera trocar 10 mm). Insert three additional trocars; see figure below for positions.
 |
Surgical Approach to the Kidney:
Start with a laterocolic incision for medial reflection of the colon. The correct layer between the meso of the colon and retroperitoneum is found most easily below the kidney. On the right side, mobilize the duodenum from the vena cava (Kocher maneuver). After sufficient colon mobilization, identify and transect the ureter at the crossing with the iliac vessels. Transect the testicular (ovarian) vein on the left side below the lower pole of the kidney, the vessel can be spared on the right side. On the left side, the aorta is followed cranially, on the right side the vena cava, until the renal hilus is reached. Lateral traction on the ureter facilitates the dissection. In case of a suspected malign tumor, lymph node dissection below the renal hilus is now possible.
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
Transection of the Renal Vessels:
Isolate the renal vessels and send suspicious lymph nodes for pathological examination. The renal vessels are transsected between ligature clips; 2–3 clips should be placed proximally. Alternatively, the renal vessels are transsected with a linear stapling device for vessels (Endo-GIA, 30–45 mm). Another option is to transsect the renal hilus en-block with a long (60 mm) Endo-GIA, see figures below.
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
Dissection of the Upper Pole:
After transection of the renal vessels, the dissection is continued along aorta/vena cava until the adrenal gland is identified. The fatty tissue between the adrenal gland and capsula adiposa is incised to spare the adrenals. Be careful not to injure the lienal vessels or the pancreatic tail.
Adrenalectomy:
If oncologically necessary, the adrenalectomy can be carried out without problems with the laparoscopic technique (en bloc with the kidney). The adrenal vessels are clipped or coagulated depending on their size.
Intact Organ Retrieval:
After complete mobilization of the kidney, the organ is deposited in a retrieval bag, which was inserted through the 10 mm trocar. Intact organ retrieval requires a sufficient muscle-spitting incision of the lower abdominal wall. Drainage of the renal fossa is optional.
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
Regional lymphadenectomy:
Lymphadenectomy is unnecessary for T1–2 tumors without suspicious lymph node enlargement, since no survival benefit could be demonstrated in a large EORTC study (Blom et al., 1999 and 2009). Some authors advocate, based on retrospective studies, lymphadenectomy if advanced tumors or enlarged lymph nodes are present. For enlarged lymph nodes, limited regional lymphadenectomy can be performed laparoscopically, or open surgery should be performed.
Morcellation:
Morcellation of the kidney spares the incision for organ retrieval and is used for benign indications. Kidney morcellation is discouraged in cases with suspected malignancy. For most reported cases with port site metastases, morcellation was used instead of intact organ retrieval.
Technical modifications:
The following modifications of the standard laparoscopic technique are sometimes used (also in combination) in laparoscopic nephrectomy:
- Hand-assisted technique: with the help of a special hand port, one hand of the surgeon can enter the abdominal cavity and help with the dissection and retraction. Disadvantageous are the high costs of the disposable item. The hand-assisted technique can also be performed without the hand port: adapt the incision for your hand size; the gas leak can be limited with moist surgical towels. The hand (port) incision is used for intact organ retrieval.
- Robot-assisted laparoscopy: the three-dimensional view, articulated instruments with several degrees of freedom, a filtered hand tremor and the ergonomic working position simplify laparoscopic surgery. For nephrectomy, the use of the robot is not justified due to the simplicity of the operation and consideration of the effort and costs.
- Single-port laparoscopy: the surgery is performed via a trocar with multiple channels and with special angulated instruments. There is also a single-port platform available for robot-assisted laparoscopy (Dobbs et al., 2020).
- NOTES: stands for Natural Orifices Transluminal Endoscopic Surgery. Few centers have demonstrated the feasibility of transvaginal NOTES nephrectomy, but there are no significant advantages and additional risks.
Care after Laparoscopic Nephrectomy
General Measures:
Early mobilization. Respiratory therapy. Thrombosis prophylaxis. Laboratory controls (Hb, creatinine). Wound inspections.
Analgesia:
Analgesics with a combination of NSAIDs and opioids.
Diet advancement:
Remove the nasogastric tube and allow small sips of clear liquids after surgery. Increase amounts of clear liquids and allow yogurt or pudding on postoperative day 1. If the patients feels well, allow small amounts of solid food (appetite driven) starting postoperative day 2.
Drains and Catheters:
Quick removal of the bladder catheter after uneventful surgery for stable patients within 12 hours, wound drainage (often unnecessary) for 1–2 days.
Complications
In principle, complication of laparoscopic nephrectomy are comparable to open nephrectomy [see section radical nephrectomy ]. In comparative studies, the laparoscopic technique reduces pain, bleeding, paralytic ileus, surgical site infections, and incisional hernia.
| Open radical nephrectomy | Index | Retroperitoneoscopic nephrectomy |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Allan u.a. 2001 ALLAN, J. D. ; TOLLEY, D. A. ;
KAOUK, J. H. ; NOVICK, A. C. ; GILL, I. S.:
Laparoscopic radical nephrectomy.
In: Eur Urol
40 (2001), Nr. 1, S. 17–23
Blom u.a. 1999 BLOM, J. H. ; POPPEL, H. van ;
MARECHAL, J. M. ; JACQMIN, D. ; SYLVESTER, R. ;
SCHRODER, F. H. ; PRIJCK, L. de:
Radical nephrectomy with and without lymph node dissection:
preliminary results of the EORTC randomized phase III protocol 30881. EORTC
Genitourinary Group.
In: Eur Urol
36 (1999), Nr. 6, S. 570–5
Blom, Jan H M; van Poppel, Hein; Maréchal, Jean M;
Jacqmin, Didier; Schröder, Fritz H; de Prijck, Linda; Sylvester, Richard &
E. O. R. T. C. Genitourinary Tract Cancer Group
Radical nephrectomy
with and without lymph-node dissection: final results of European
Organization for Research and Treatment of Cancer (EORTC) randomized phase
3 trial 30881.
Eur Urol, 2009, 55, 28-34.
Desai u.a. 2005 DESAI, M. M. ; STRZEMPKOWSKI,
B. ; MATIN, S. F. ; STEINBERG, A. P. ; NG, C. ;
MERANEY, A. M. ; KAOUK, J. H. ; GILL, I. S.:
Prospective randomized comparison of transperitoneal versus
retroperitoneal laparoscopic radical nephrectomy.
In: J Urol
173 (2005), Nr. 1, S. 38–41
Dobbs RW, Halgrimson WR, Talamini S, Vigneswaran HT, Wilson JO, Crivellaro S. Single-port robotic surgery: the next generation of minimally invasive urology. World J Urol. 2020 Apr;38(4):897-905. doi: 10.1007/s00345-019-02898-1. Epub 2019 Aug 28.
 Deutsche Version: Laparoskopische Nephrektomie
Deutsche Version: Laparoskopische Nephrektomie
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.