You are here: Urology Textbook > Ureters > Megaureter
Megaureter: Symptoms, Diagnosis and Treatment
Definition of Megaureter
A megaureter is an anomaly with a dilated ureter of more than 7–8 mm (Shokeir and Nijman, 2000) (Mouriquand and Wilcox, 1998) (EAU Guidelines); the further division is made according to the cause:
Primary Obstructive Megaureter (POM):
Primary obstructive megaureter is a congenital ureteral dilatation caused by an aperistaltic ureteral segment at the ureterovesical junction. An embryological stop of the ureter development causes disorientation of the muscle fibers and impaired urine flow.
 |
Secondary Obstructive Megaureter:
Increased intravesical pressure, increased bladder wall tension, and scarring lead to the obstruction of the uretero-vesical junction.
Refluxing Megaureter:
Vesicoureteral reflux causes dilatation of the ureter.
Idiopathic (non-obstructive and non-refluxing) Megaureter:
Most newborn megaureters are idiopathic; the cause often remains unclear. Increased urine production, a delay of ureteral maturation, or subclinical obstruction may contribute to the development of a megaureter.
Refluxing and Obstructive Megaureter:
The megaureter is caused by the combination of distal stenosis and vesicoureteral reflux (rare).
Epidemiology of Megaureter
Megaureters account for 20% of cases with prenatally diagnosed hydronephrosis.
Diagnosis of Megaureter
Ultrasonography:
Ultrasound imaging of kidney, ureter, and bladder may differentiate between ureteropelvic junction obstruction and megaureter. The ureter in children is usually less than 5 mm wide.

|
Intravenous Urography:
Urography is also well suited for the differential diagnosis between ureteropelvic junction obstruction and megaureter. Furthermore, imaging provides information about split kidney function.
Voiding Cystourethrogram:
A voiding cystourethrogram confirms or excludes vesicoureteral reflux or posterior urethral valves.
Renal Scintigraphy:
Renal scintigraphy determines split renal function and distinguishes between real obstruction and idiopathic (non-obstructive) megaureter. The nuclide wash-out 20 minutes after furosemide injection should be more than 50% to rule our significant obstruction.
Retrograde Pyelography and Ureteroscopy:
Retrograde pyelography and URS are indicated for unclear cases, e.g., to rule out malignancy or ureterolithiasis after diagnosis in adult life [fig. primary obstructive megaureter].

|
Whitaker Perfusion Test:
With the help of a percutaneous nephrostomy, the renal pelvic pressure is determined during a flow rate of 10 ml/min. A Whitaker test is indicated if renal scintigraphy is unclear, especially in poor kidney function.
Treatment of Megaureter
Treatment of Obstructive Megaureter:
The primary obstructive megaureter in children has a relevant spontaneous healing rate. Indications for an intervention (balloon dilatation or surgery) are a significant obstruction, recurrent febrile UTI, or progressive loss of kidney function.
Balloon dilatation:
Balloon dilatation and temporary DJ ureteral stent over several months, success rates of 25–90% are reported (Kassite et al., 2018).
|
|
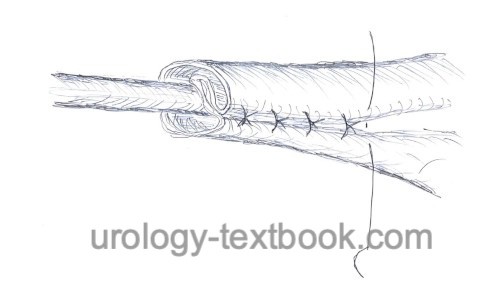
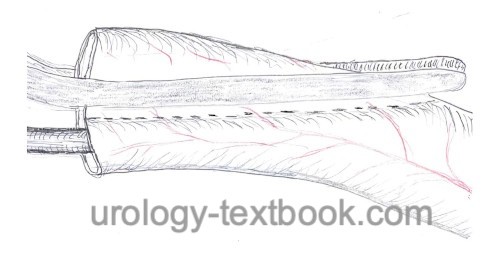
Surgery:
Surgical treatment of an obstructive megaureter includes excision of the narrow ureteral segment, ureter modellage (folding or vessel-sparing longitudinal resection, see figures above), and ureteroneocystostomy.
Treatment of Secondary Obstructive Megaureter:
Treatment of the underlying disease should be sufficient.
Refluxing Megaureter:
Please see section vesicoureteral reflux, in most cases medical management is sufficient. If surgery is necessary, perform ureteroneocystostomy with ureter modellage depending on the ureter's diameter.
Idiopathic Megaureter:
Observation and conservative treatment (of e.g., infections) is sufficient.
| Diseases of the ureters | Index | Retrocaval ureter |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
EAU guidelines: Paediatric Urology
I. Kassite et al., “High Pressure Balloon Dilatation of Primary Obstructive Megaureter in Children: A Multicenter Study.,” Front Pediatr, vol. 6, p. 329, 2018, doi: 10.3389/fped.2018.00329.
Shokeir und Nijman 2000 SHOKEIR, A. A. ; NIJMAN,
R. J.:
Primary megaureter: current trends in diagnosis and treatment.
In: BJU Int
86 (2000), Nr. 7, S. 861–8
Wilcox und Mouriquand 1998 WILCOX, D. ;
MOURIQUAND, P.:
Management of megaureter in children.
In: Eur Urol
34 (1998), Nr. 1, S. 73–8
 Deutsche Version: Megaureter
Deutsche Version: Megaureter
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.