You are here: Urology Textbook > Surgery (procedures) > Mid-urethral sling
Mid-Urethral Sling: Technique Step-by-Step and Complications
Indications for Mid-Urethral Slings
Stress urinary incontinence in women, especially with insufficiency of the anterior compartment of the pelvic floor with a hypermobile urethra.
Contraindications
- Existing or planned pregnancy
- Incomplete bladder emptying
- Untreated urge incontinence
- Stress incontinence due to other causes than anterior compartment insufficiency
- Coagulation disorders
- Urinary tract infection
- Further contraindications depend on the surgical risk due to the comorbidity of the patient.
Surgical Technique (Step-by-Step) of the Mid-Urethral Sling Procedure
Sling material:
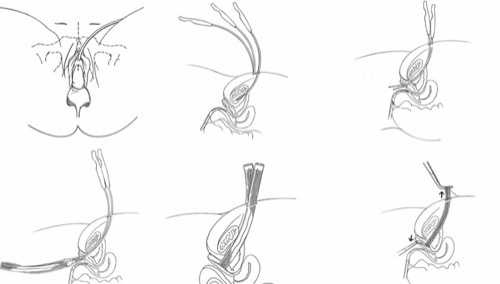
Monofilament and widely porous polypropylene mesh with 1 cm width and 40 cm length, both ends fixed to a trocar [fig. mid-urethral sling].
Preoperative patient preparation:
Vaginal estrogen treatment for several weeks before surgery. Exclusion or treatment of a urinary tract infection. Perioperative antibiotic prophylaxis. General or spinal anesthesia, but the procedure can also be performed under local anesthesia. Lithotomy position. Vaginal examination and cystoscopy. Insert a transurethral catheter with a rigid catheter guide to allow movement of the urinary bladder and urethra.
Vaginal dissection:
Inject at least 50 ml of normal saline or dilute lidocaine at the planned vaginal incision, around the urethra, and along the intended path for the trocars. Hydrodissection facilitates the preparation and reduces the risk of urinary bladder perforation. Grasp the vaginal wall just below the urethral meatus with upward traction to improve visualization of the surgical field. Perform a sagittal incision (1.5 cm length) of the anterior vaginal wall along the urethra, at least 1.5 cm distal to the bladder neck. Gentle pulling of the transurethral catheter helps to visualize the bladder neck. Use sharp (scissors) and blunt (finger) dissection to reach the inferior ramus of the pubis.
Retropubic sling implantation:
The trocar of the sling is advanced finger-guided paraurethrally through the vaginal incision to the inferior ramus of the pubis. The bladder is deflected away from the trocar path using the rigid catheter guide. The trocar is advanced through the endopelvic fascia into the retropubic space, staying close to the pubic bone to avoid injury of the bladder. The trocar exits via a small paramedian suprapubic skin incision. Secure the sling with a clamp. The same procedure is performed on the opposite side. Exclude bladder injury with a cystoscopy.
Other systems (e.g., Sparc from AMS) use an outside-in technique: the trocar needle is passed through a suprapubic incision to the vaginal incision, and the sling is anchored to the trocar and then pulled through [fig. outside-in technique].
 |
Adjustment of the sling tension:
The sling should be without tension with an empty bladder, and a pair of scissors should fit easily between the urethra and the sling. The effect of the sling may checked with bladder filling and applying pressure (coughing of the patient, suprapubic manual pressure). If the band is correctly positioned, remove the plastic sheath, and cut the abdominal ends below the skin level. Close the abdominal (4-0) and vaginal (2-0) incisions with interrupted synthetic absorbable sutures.
Transobturator mid-urethral sling:
Transobturator mid-urethral slings were developed as a technical alternative to reduce the associated complications of retropubic slings (bladder or bowel injury, urinary retention). Different systems are on the market; basic technical differences exist regarding the direction of trocar passage (inside-out or outside-in) [fig. transobturator sling].
 |
Minimally invasive alternatives:
Single-incision slings are implanted via the vaginal incision, the slings are anchored in the paraurethral tissue and pelvic floor muscles [fig. short mid-urethral devices].
Postoperative Care after Mid-Urethral Sling Procedures
Bladder catheter:
Remove the foley catheter after 2–24 hours, unless significant hematuria suggests bladder perforation. Check postvoid residual volume after voiding trial. Sling loosening (in general anesthesia) is necessary for patients with urinary retention.
Complications
- De novo urge symptoms or dyspareunia (up to 10%).
- Numbness and pain of the groin or thigh in 10% (with transobturator slings)
- Subvesical obstruction with urinary retention (more common with retropubic slings).
- Persistent incontinence in < 10% (more common with transobturator slings)
- Urethral injury
- Uncommon: injury to the bladder, iliac vessels, or bowel (with retropubic implantation).
- Vaginal, vesical, or urethral erosion of the sling, in the long term up to 12%.
| TURB | Index | Sectio alta and cystolithotomy |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
V. Alexandridis, A. Lundmark Drca, M. Ek, and W. S. derberg, “Retropubic slings are more efficient than transobturator at 10-year follow-up: a Swedish register-based study.,” Int Urogynecol J., vol. 34, no. 6, pp. 1307–1315, 2023.
A. Mostafa, C. P. Lim, L. Hopper, P. Madhuvrata, and M. Abdel-Fattah, “Single-incision mini-slings versus standard mid-urethral slings in surgical management of female stress urinary incontinence: an updated systematic review and meta-analysis of effectiveness and complications.,” Eur Urol, vol. 65, no. 2, pp. 402–427, 2014.
Latthe, P. M.; Singh, P.; Foon, R. & Toozs-Hobson, P.
Two
routes of transobturator tape procedures in stress urinary incontinence: a
meta-analysis with direct and indirect comparison of randomized trials.
BJU
Int, 2010, 106, 68-76
Liedl u.a. 2005 LIEDL, B. ; SCHORSCH, I. ;
STIEF, C.:
[The development of concepts of female (in)continence.
Pathophysiology, diagnostics and surgical therapy].
In: Urologe A
44 (2005), Nr. 7, S. W803–18; quiz W819–20
Ward, K. L.; Hilton, P.; K., U. & Group, I. T. T.
Tension-free
vaginal tape versus colposuspension for primary urodynamic stress
incontinence: 5-year follow up.
BJOG, 2008, 115,
226-233
 Deutsche Version: Alloplastische vordere Vaginalbänder
Deutsche Version: Alloplastische vordere Vaginalbänder
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.