You are here: Urology Textbook > Penis > Sexually transmitted diseases & Non-gonococcal urethritis
Non-Gonococcal Urethritis (NGU)
Review-Literature: (CDC Guidelines, 2021) (Schneede et al., 2003).
Definition
Non-gonococcal urethritis is an infectious urethritis that is not caused by Neisseria gonorrhoeae.
Epidemiology of Non-gonococcal Urethritis
The incidence of NGU is increasing and is now more frequent than gonorrheal urethritis.
Incidence of chlamydia infection
The epidemiological figures for chlamydia infection vary greatly in Europe; in countries with screening, the incidence is 300–500/100,000. The estimated prevalence in young people (14–24 years) in the USA and Europe is 2–7%; the majority are asymptomatic.
Causes (Pathogens) of Non-Gonococcal Urethritis
Chlamydia trachomatis:
Chlamydia trachomatis is a gram-negative obligate intracellular bacteria and the most frequent pathogen of NGU. Urethritis is caused by serotypes D–K.
Morphology:
The extracellular forms of Chlamydia are elementary bodies (diameter 0.3 μm); the intracellular multiplication creates intracellular inclusion bodies.
Mycoplasma:
Mycoplasma causes 20% of NGU. Important species are Mycoplasma genitalis and Ureaplasma urealyticum. Mycoplasma grows optional anaerobic and as extracellular parasites on epithelial cells.
Morphology:
Mycoplasmas are spherical to filamentous cells without cell walls; for microscopy, use Giemsa staining. Size between 0.1–0.6 μm.
Gram-positive bacteria:
Enterococci in 15%, Streptococci in 12%, Staphylococcus aureus in 5%.
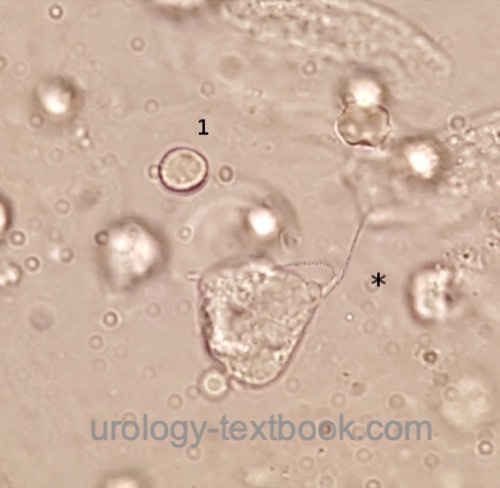
Trichomonas vaginalis:
Trichomonas vaginalis is an parasitic flagellated protozoan and a rare cause of urethritis (<1%). It is very easily detectable in vaginal secretions, and occasionally seen in urine sediment, see fig. Trichomonas vaginalis.
 |
Further causes:
Unknown etiology in 20–30%. Seldom viral urethritis, mechanical causes (iatrogen, or (self) manipulation).
Signs and Symptoms
Urethritis:
The incubation period is 1–5 weeks. Men complain of glassy or purulent discharge from the urethra, dysuria, and burning in the urethra. Women complain of vaginal discharge, dysuria, and abdominal pain (which is a sign of progression to pelvic inflammatory disease). The extent of the symptoms is very variable, and many are asymptomatic.
Complications:
Ascending infections may lead to complications: epididymitis in men and pelvic inflammatory disease (PID) in women. Complications may cause infertility in men and women, which is best documented for PID. The risk for tubal occlusion is around 10\% after the first PID, increasing with the number of episodes. After PID, there is also an increased risk for ectopic pregnancies. Neonates may be infected by their mother (chlamydial conjunctivitis or pneumonia).
Reiter syndrome:
Reiter syndrome is a HLA-B-27-associated autoimmune disease with arthritis, conjunctivitis, balanitis, fever and rashes with cornification at the palms and soles (fig. keratoderma blennorrhagicum). The symptoms develop after a urethritis or gastroenteritis. Due to a mixed infection, the Reiter syndrome is also possible due to gonorrhea.
 |
Fitz-Hugh-Curtis syndrome:
Fitz-Hugh-Curtis syndrome is an ascending pelvic inflammatory disease with peritoneal infection. Typical is right-sided abdominal pain due to infection of the hepatic peritoneum (perihepatitis).
Diagnosis
Indications for microbiological testing in men:
Urethral discharge, diagnosis of any other STI, sexual partners with STI, and acute epididymitis in a male under 40 years.
Indications for microbiological testing in women:
Vaginal discharge with risk factors for STI (history, age), diagnosis of any other STI, sexual partners of patients with STI, and acute pelvic inflammatory disease.
Swab tests:
The urethral swab is ideally done after a longer pause in micturition. Further pathogen collection from the anus, pharynx, and cervix depends on history and symptoms. The microbiological diagnosis is possible with different techniques:
NAAT:
With the help of a NAAT (Nucleic Acid Amplification Test), gonococci, chlamydia and mycoplasma are detected with high sensitivity and specificity.
Microscopic diagnosis:
Two microscope slides for Gram stain (gonococcus) and Giemsa stain (Chlamydia) are prepared if a microscopic pathogen detection is sought.
Test of the sexual partner:
To avoid a ping-pong infection, a detailed history and examination of any sexual partner is necessary.
Urin analysis:
After the urethral swab, urine for culture is collected.
Serological tests:
Other STDs like syphilis, hepatitis, and HIV should be tested.
Notifiable disease:
Chlamydia is a notifiable disease in some countries, e.g., Australia.
Treatment of Non-gonococcal Urethritis
Standard treatment:
Standard treatment for non-gonococcal urethritis is doxycyclin 100 mg 1-0-1 p.o. over 7 days or azithromycin 1–2 g p.o. once. If gonococcal infection is possible, add ceftriaxon 1 g i.m. once and prefer azithromycin.
Alternative Treatment:
Levofloxacin 500 mg p.o. 1-0-0 or ofloxacin 300 mg p.o. 1-0-1 or erythromycin 500 mg p.o. 1-1-1-1 for seven days.
Follow-up and test of cure (TOC):
Sexual abstinence until antibiotic therapy is finished. A TOC is not recommended, unless symptoms persist or reinfection is suspected.
Prevention:
Use of condoms, treatment with intravaginal nonoxynol-9 containing spermicides, antibiotic prophylaxis after sexual intercourse, treatment of newborn eyes with an antibiotic ointment containing silver nitrate, erythromycin, or tetracycline (Credé prophylaxis).
| Gonorrhea | Index | Syphilis |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Center for Disease Control and Prevention: “Sexually Transmitted Infections (STI) Treatment Guidelines,” 2021. [Online]. Available: https://www.cdc.gov/std/treatment-guidelines/STI-Guidelines-2021.pdf
EAU Guidelines "Urological Infections,” Available: https://uroweb.org/guidelines/urological-infections/.
IUSTI Guideline on the management of Chlamydia trachomatis infections: https://iusti.org/wp-content/uploads/2019/12/Chlamydia2015.pdf
RKI Ratgeber zu Chlamydien Infektionen: https://www.rki.de/DE/Content/Infekt/EpidBull/Merkblaetter/Ratgeber_Chlamydiosen_Teil1.html
 Deutsche Version: nichtgonorrhoische Urethritis.
Deutsche Version: nichtgonorrhoische Urethritis.