You are here: Urology Textbook > Surgery (procedures) > Open pyeloplasty
Open Pyeloplasty: Anderson-Hynes Technique (Step by Step)
Indications for Pyeloplasty
Pyeloplasty is the surgical therapy for ureteropelvic junction obstruction:
- with scintigraphic evidence of obstruction
- with decreasing (but sufficient) renal function of the affected kidney
- with clinical symptoms (flank pain, nephrolithiasis, or recurrent infections)
Pyeloplasty is possible open-surgically and laparoscopically (see next section); open surgery is recommended if the patient has undergone previous perirenal surgery.
Contraindications for Pyeloplasty
Nonfunctioning kidney (under 20% of total renal clearance). Coagulation disorders. The other contraindications depend on the surgical risk due to the patient's comorbidity, the renal function of the contralateral kidney, and the surgical procedure's impact on the patient's quality of life.
Dismembered Pyeloplasty: Anderson-Hynes Technique
 |
Preoperative Patient Preparation
- Exclude or treat urinary tract infection
- Insert a DJ ureter stent and ensure the diagnosis with retrograde pyelography
- Perioperative antibiotic prophylaxis
- Insertion of a transurethral catheter
- Consider epidural anesthesia
Surgical Approach via a Flank Incision
A flank incision is the most common surgical approach to the kidney for open pyeloplasty in adults. In children, an anterior subcostal muscle-splitting approach is preferable. See also the following section for laparoscopic pyeloplasty.
The kidney is completely exposed without opening the peritoneum. Identify the proximal ureter and mark it with a vessel loop. Open the renal fascia and dissect the renal pelvis on the anterior and dorsal sides.
Steps of Anderson-Hynes Dismembered Pyeloplasty
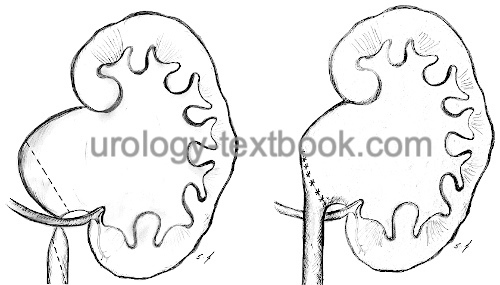
Dismembered pyeloplasty, described by Anderson and Hynes in 1949, is the method of choice if a crossing vessel is identified as the cause of the UPJ obstruction and probably for most other indications. Traction sutures are placed at the renal pelvis. Excise the UPJ obstruction with, if necessary, excess renal pelvis (reduction pyeloplasty) (reduction pyeloplasty). The ureter is spatulated along the lateral wall (2–3 cm) [fig. dismembered pyeloplasty]. The ureter is repositioned concerning the crossing vessel, resulting in an anastomosis ventral of the crossing vessels.
The anastomosis between the ureter and renal pelvis is done with fine PDS or Vicryl sutures (4-0, in children even finer). First, the cranial part of the opened renal pelvis is closed with a running suture. The caudal part of the renal pelvis (2–3 cm) is left open for the anastomosis with the ureter. The ureter is anastomosed with either a running or interrupted suture to the caudal portion of the renal pelvis. Before the last sutures are done, the position of the ureteral stent is controlled.
Spiral flap pyeloplasty:
The Culp-De Weerd technique is an option in recurrent surgery with a large ectatic renal pelvis [fig. spiral flap pyeloplasty]. A flap from the renal pelvis is used to bridge the UPJ stenosis or a scarred stricture until the proximal ureter.
 |
Drainage:
Drainage of the renal fossa is recommended.
Care after Pyeloplasty
General measures:
Early mobilization, thrombosis prophylaxis, respiratory therapy, laboratory tests (hemoglobin, creatinine), regular physical examination of the abdomen and incision wound.
Analgesia:
Analgesics with a combination of NSAIDs and opioids. Peridural anesthesia facilitates postoperative pain management.
Drains and catheters:
Remove the retroperitoneal drainage if the daily drainage is below 50 ml. The bladder catheter stays additional 1–2 days or 3–5 days in total, and the ureteral stent for 2–4 weeks.
Complications of Pyeloplasty
The success rate of renal pyeloplasty (sufficient urine drainage in the long term) is high, at over 95% for primary surgery patients. The success rate for recurrent surgery is significantly lower at 84% (Inagaki et al., 2005).
- Insufficiency of the anastomosis: urinoma, urinary peritonitis, recurrent ureteral stricture, loss of renal function.
- General surgical risks: Bleeding, wound infection, urinary tract infection, injury to neighboring organs (liver, spleen, intestine and pancreas). Incisional hernia (due to subcostal nerve injury).
| Urologic Surgery | Index | Prostate biopsy |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
ANDERSON, J. C. & HYNES, W.
Retrocaval ureter; a case diagnosed pre-operatively and treated successfully by a plastic operation.
Br J Urol, 1949, 21, 209–214
Culp, O. S. & Deweerd, J. H.
A pelvic flap
operation for certain types of ureteropelvic obstruction; observations
after two years' experience.
J Urol, 1954, 71,
523-529
J. A. Smith, S. S. Howards, G. M. Preminger, and R. R. Dmochowski, Hinman’s Atlas of Urologic Surgery Revised Reprint. Elsevier, 2019.
C. Radmayr, G. Bogaert, H. S. Dogan, and S. Tekgül, “EAU Guidelines: Paediatric Urology.” [Online]. Available: https://uroweb.org/guidelines/paediatric-urology/
 Deutsche Version: Technik der offen-chirurgischen Nierenbeckenplastik
Deutsche Version: Technik der offen-chirurgischen Nierenbeckenplastik