You are here: Urology Textbook > Surgery (procedures) > Retroperitoneal Lymphadenectomy
Retroperitoneal Lymphadenectomy (RLA): Surgical Technique and Complications
Indication for retroperitoneal lymphadenectomy
RLA is a treatment option in different stages of germ cell tumors:
- Nonseminoma Stage I: nerve-sparing modified RLA is an option in nonseminoma stage I and an alternative to prophylactic chemotherapy or active surveillance.
- Tumor Marker Negative Nonseminoma Stage IIA: nerve-sparing RLA is recommended for tumor markers negative nonseminoma stage IIA. Before surgery, imaging and tumor marker should be repeated after six weeks. RLA is indicated for persistence or progression of the lymph nodes without tumor marker elevation.
- Residual Mass after Chemotherapy with Normalized Tumor Markers: retroperitoneal lymphadenectomy should be performed for residual masses of over 1–2 cm in size (nonseminoma) and over 3 cm in size (seminoma). The dissection field depends on the extent of the metastases before chemotherapy.
Contraindications for Retroperitoneal Lymphadenectomy
Uncorrected coagulation disorders. Significant medical comorbidities preventing major abdominal surgery. Preoperatively, complete resection of the tumor manifestation should appear possible. No metastases in other localization or rising/elevated tumor markers requiring additional chemotherapy.
Surgical Technique of Retroperitoneal Lymphadenectomy
Preoperative Patient Preparation:
Start with a clear liquid diet 24 hours before the planned operation, which leads to emptying the small bowel system from solid debris. Clear soups, plenty of sweet drinks, and high-energy tube feedings without fibers are permitted. The evening before surgery, an enema is used to clean the rectum.
On the day of surgery: supine positioning with a slight extension of the lumbar spine, perioperative antibiotic prophylaxis, general anesthesia with additional PDA, perioperative bladder catheter, and nasogastric tube.
Transperitoneal Surgical Approach:
Midline laparotomy from the xiphoid process to the lower abdomen (between the navel and symphysis) depending on the body mass index. Dissect the ligament teres hepatis and free the liver from the diaphragm by incision of the falciform ligament. The ascending colon and caecum are mobilized by incision of the peritoneum starting laterocolic and along the small intestinal meso to the ligament of Treitz. The ascending colon and the complete mesentericum of the small intestine are detached from the retroperitoneum and displaced cranially. With the help of the Kocher maneuver, the duodenum and part of the pancreas are reflected to the left until the renal veins become visible as cranial borders of the dissection area. Carefully pad the intestinal pack with moist abdominal towels and store it on the thorax; regularly inspect for sufficient blood flow (ischemia due to compression/tension of the superior mesenteric vessels).
Thoracoabdominal Surgical Approach:
Seldom needed for the removal of enlarged retrocrural lymph nodes.
Template for Nerve-Sparing Retroperitoneal Lymphadenectomy:
A nerve-sparing dissection field for right or left testicular tumors respects the probability of lymph node metastases and reduces the frequency of retrograde ejaculation. It is necessary to identify the sympathetic ganglia and to protect the exiting sympathetic nerve fibers crossing the dissection field.
The frozen section diagnosis of the removed lymph nodes differs between centers. Most open surgical and a few laparoscopic centers send the lymph nodes to a frozen section examination. If lymph node metastases are diagnosed, the contralateral lymph nodes are removed in the contralateral dissection field (bilateral nerve-sparing lymphadenectomy). The remaining centers do not perform intraoperative frozen section examinations; adjuvant chemotherapy is recommended in case of lymph node metastases.
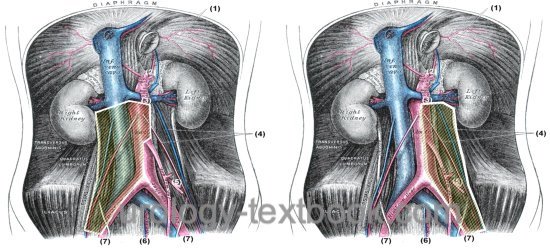 |
Template borders for Right-Sided Testicular Tumors:
- Right: lateral border of the testicular vein and ureter.
- Cranial: renal vein
- Left: left lateral border of the aorta, above the inferior mesenteric artery the interaortocaval lymph nodes are removed in addition.
- Caudal: cranial border of the iliac artery, dissection ends at the crossing of the ureter with the iliac vessels.
Template borders for Left-Sided Testicular Tumors:
- Left: lateral border of the testicular vein and ureter
- Cranial: renal vein
- Right: medial border of the aorta (without interaortocaval lymphe nodes).
- Caudal: cranial border of the iliac artery, dissection ends at the crossing of the ureter with the iliac vessels.
Dissection Technique for Radical Retroperitoneal Lymphadenectomy:
Bilateral radical retroperitoneal lymphadenectomy is indicated in advanced germ cell cancer with initial bilateral metastases and residual tumor masses after chemotherapy. Use the split-and-roll technique to remove all lymph nodes along the large vessels. Firstly, the lymphatic tissue is split on the aorta and on the inferior vena cava (split). Then, the large vessels are rolled to the side, and the lumbar arteries and lumbar veins are ligated or clipped (roll). The aorta and the inferior vena cava are now completely dissected and can be lifted with vessel loops from the retroperitoneal lymphatic tissue. The lymphatic tissue is removed, and once again, it is necessary to ligate or clip the lumbar arteries and veins. If possible, the sympathetic ganglia and emerging nerve fibers are identified and spared.
Wound closure:
Careful heomastasis. Insert a drain. See section midline laparotomy for wound closure.
Technical Modifications:
Laparoscopic RPLND is an option in expert hands to shorten hospitalization (Schwartz et al., 2010). The complex procedure is facilitated by the robotic-assisted technique (Garg et al., 2023). Prospective trials comparing the oncological outcome are not available.
Postoperative Care after Retroperitoneal Lymphadenectomy
General measures:
Early mobilization. Respiratory therapy. Thrombosis prophylaxis. Laboratory controls (Hb, creatinine). Wound inspections.
Analgesia:
With epidural anesthesia, and, if necessary, with a combination of NSAIDs and opioids.
Diet advancement:
Remove the nasogastric tube and allow small sips of clear liquids after surgery. Increase amounts of clear liquids and allow yogurt or pudding on postoperative day 1. If the patients feels well, allow small amounts of solid food (appetite driven) starting postoperative day 2.
Drains and catheters:
Quick removal of the bladder catheter after uneventful surgery for stable patients within 12 hours. Remove wound drainage after feeding with a fat-containing diet is tolerated and no fat-containing drainage (chylous leakage) is seen.
Complications of Retroperitoneal Lymphadenectomy
Post-chemotherapy RLA harbors significantly more complications than primary RLA in stage I–II germ cell tumor (Baniel et al., 1995) (Baniel et al., 1994).
Retrograde Ejaculation After Retroperitoneal Lymphadenectomy:
In order to avoid retrograde ejaculation, it is important to respect the modified dissection field (see above) and to identify and preserve the sympathetic ganglia and emerging nerve fibers. Nerve-sparing is often not possible in surgery after chemotherapy, and retrograde ejaculation is a significant risk. The results are more favorable for the primary nerve-sparing RLA with less than 5% retrograde ejaculation.
Injury to Neighboring Organs
Paralytic ileus, bowel injury, peritonitis, pancreatic tail injury with formation of a pancreatic fistula. Chylous fistula due to injury of intestinal lymphatic vessels. Injury to liver or spleen, depending on the side of surgery.
General Complications:
Bleeding, wound infection, thrombosis, pulmonary embolism, atelectasis, pneumonia, and acute renal failure.
Mortality:
0.8% for RLA after chemotherapy.
| Urologic Surgery | Index | Hydrocelectomy |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
J. Baniel, R. S. Foster, R. G. Rowland, R. Bihrle, und J. P. Donohue.
Complications of primary retroperitoneal lymph node dissection.
J Urol, 152 (2 Pt 1): 424–427, Aug 1994.
J. Baniel, R. S. Foster, R. G. Rowland, R. Bihrle, und J. P. Donohue.
Complications of post-chemotherapy retroperitoneal lymph node
dissection.
J Urol, 153 (3 Pt 2): 976–980, Mar 1995.
H. Garg et al., “Robot-assisted retroperitoneal lymph node dissection: a systematic review of perioperative outcomes.,” BJU int., vol. 132, no. 1, pp. 9–30, 2023, doi: 10.1111/bju.15986.
H. W. Herr, J. Sheinfeld, H. S. Puc, R. Heelan, D. F. Bajorin, P. Mencel, G. J.
Bosl, und R. J. Motzer.
Surgery for a post-chemotherapy residual mass in seminoma.
J Urol, 157 (3): 860–862, Mar 1997.
J. A. Smith, S. S. Howards, G. M. Preminger, and R. R. Dmochowski, Hinman’s Atlas of Urologic Surgery Revised Reprint. Elsevier, 2019.
M. J. Schwartz and L. R. Kavoussi, “Controversial technology: the Chunnel and the laparoscopic retroperitoneal lymph node dissection (RPLND).,” BJU int., vol. 106, no. 7, pp. 950–959, 2010, doi: 10.1111/j.1464-410X.2010.09659.x.
 Deutsche Version: Retroperitoneale Lymphadenektomie
Deutsche Version: Retroperitoneale Lymphadenektomie
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.