You are here: Urology Textbook > Surgery (procedures) > Retroperitoneoscopic nephrectomy
Surgical Steps and Complications of Retroperitoneoscopic Nephrectomy
Retroperitoneoscopic nephrectomy has clear advantages over open nephrectomy (less bleeding, postoperative pain, paralytic ileus, wound infection, and incisional hernia) and leads to a faster postoperative recovery of the patient.
Indications for Retroperitoneoscopic Nephrectomy
Benign diseases:
Nonfunctioning kidney with symptoms (e.g., bleeding, recurrent infections, nephrolithiasis, hydronephrosis, flank pain or renal hypertension).
Malignant diseases:
Renal cell carcinoma (up to 8 cm in size, depending on location) if partial nephrectomy is not feasible.
Contraindications for Retroperitoneoscopic Nephrectomy
Coagulation disorders. Do not perform radical nephrectomy if partial nephrectomy is technically possible, especially in patients with single kidneys, chronic kidney disease, bilateral renal cell cancer, or hereditary renal cell cancer. Choose the open surgical technique for large tumors (size >8 cm depending on location), lymph node metastasis, or vein thrombus. Choose the laparoscopic or open surgical approach after major retroperitoneal surgery of the same side. The other contraindications depend on the surgical risk due to the patient's comorbidity, the renal function of the contralateral kidney, and the surgical procedure's impact on the patient's life expectancy.
Surgical Technique of Retroperitoneoscopic Nephrectomy
Preoperative Preparations:
- Enema on the evening before surgery, bowel preparation is unnecessary.
- Perioperative placement of a bladder catheter and gastric tube.
- Perioperative antibiotic prophylaxis is needed if risk factors for surgical site infections are present or if the urinary tract is planned to be opened.
- Insert a transurethral catheter and gastric feeding tube during surgery.
Patient Positioning:
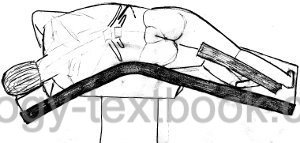
The patient is placed in a lateral position on a flexed operation table. The positioning on a vacuum mattress enables a secure fixation of the patient, even if the operation table has to be tilted.
 |
Surgical approach to the retroperitoneum:
Create a 2 cm incision in the area of the trigonum lumbale (below the tip of the 12th rib). Push aside the musculature with small Langenbeck retractors and incise the fascia thoracolumbalis. Blunt finger dissection enlarges the retroperitoneal cavity. Further enlargement is possible with a special balloon dilator, allowing dilation under direct vision. Insert a Hasson optic trocar, carbon dioxide (CO$_2$) is used for the distension of the retroperitoneal cavity, and the working pressure is usually between 12–15 mmHg. Two more trocars are inserted without entering the peritoneal cavity. If space is an issue, a trocar can be placed between the 11th and 12th ribs. Incise the fascia renalis near the psoas muscle, further blunt development of the retroperitoneal cavity is possible. Next landmarks are the arcuate ligaments of the diaphragm (cranial) and ureter and gonadal vein (caudal).
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
Dissection of the renal hilus:
Start with a blunt preparation between the renal fascia and the psoas muscle and identify the aorta or vena cava. The gonadal vessels (left side) and ureter (both sides) are clipped and transsected early. The renal artery is dorsal to the renal vein and the first vessel to be seen from the camera view. Divide the renal vessels using a linear stapling device or locking clips for large vessels.
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
Dissection of the upper pole:
Mobilize the ventral kidney surface from the peritoneum. Continue with the dissection along the aorta/vena cava until the adrenal gland is identified. Incise the fatty tissue between the adrenal gland and capsula adiposa to spare the adrenals. Be careful not to injure the lienal vessels or the pancreatic tail.
Organ retrieval:
For benign indications, the kidney is mobilized along the organ capsule. After complete mobilization, the organ is deposited in a big retrieval bag. Intact organ retrieval requires a sufficient muscle-spitting incision. Morcellation of the kidney can avoid an incision for patients with benign kidney disease. The drainage of the renal fossa is unnecessary after uncomplicated surgery.
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
Technical modifications:
The following modifications of the standard retroperitoneoscopic technique are sometimes used (also in combination) for retroperitoneoscopic nephrectomy:
- Robot-assisted laparoscopy: the three-dimensional view, articulated instruments with several degrees of freedom, a filtered hand tremor and the ergonomic working position simplify laparoscopic surgery. For nephrectomy, the use of the robot is not justified due to the simplicity of the operation and consideration of the effort and costs.
- Single-port laparoscopy: the surgery is performed via a trocar with multiple channels and with special angulated instruments. There is also a single-port platform available for robot-assisted laparoscopy (Dobbs et al., 2020).
Care after Retroperitoneoscopic Nephrectomy
General Measures:
Early mobilization. Respiratory therapy. Thrombosis prophylaxis. Laboratory controls (Hb, creatinine). Wound inspections.
Analgesia:
Analgesics with a combination of NSAIDs and opioids.
Diet advancement:
Remove the nasogastric tube after surgery and allow small sips of clear liquids. On the first postoperative day, start with yogurt, pudding, and small amounts of solid food (appetite-driven).
Drains and Catheters:
Quick removal of the foley catheter after uneventful surgery for stable patients within 12 hours, wound drainage (often unnecessary) for 1–2 days.
Complications
In principle, complications of retroperitoneoscopic nephrectomy are comparable to open nephrectomy [see section radical nephrectomy ]. In comparative studies, the retroperitoneoscopic technique reduces pain, bleeding, paralytic ileus, surgical site infections, and incisional hernia.
| Open radical nephrectomy | Index | Open partial nephrectomy |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Desai u.a. 2005 DESAI, M. M. ; STRZEMPKOWSKI,
B. ; MATIN, S. F. ; STEINBERG, A. P. ; NG, C. ;
MERANEY, A. M. ; KAOUK, J. H. ; GILL, I. S.:
Prospective randomized comparison of transperitoneal versus
retroperitoneal laparoscopic radical nephrectomy.
In: J Urol
173 (2005), Nr. 1, S. 38–41
Dobbs RW, Halgrimson WR, Talamini S, Vigneswaran HT, Wilson JO, Crivellaro S. Single-port robotic surgery: the next generation of minimally invasive urology. World J Urol. 2020 Apr;38(4):897-905. doi: 10.1007/s00345-019-02898-1. Epub 2019 Aug 28.
 Deutsche Version: Retroperitoneoskopische Nephrektomie
Deutsche Version: Retroperitoneoskopische Nephrektomie
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.