You are here: Urology Textbook > Bladder > Stress urinary incontinence in women > Stress urinary incontinence in women > treatment
Treatment of Stress Urinary Incontinence in Women
- Stress urinary incontinence in women: definition and etiology
- Stress urinary incontinence: symptoms and diagnostic workup
- Stress urinary incontinence: medical and surgical treatment
Treatment of Stress Urinary Incontinence (SUI)
Conservative treatment of Stress Urinary Incontinence
Weight reduction, regular micturition to avoid a full bladder, pelvic floor exercises, and topical (vaginal) estrogen treatment are conservative treatment options for stress urinary incontinence.
Vaginal estrogen therapy:
Vaginal estrogen therapy should be offered to every postmenopausal woman with stress urinary incontinence. Dosage: 0,03–0,5 mg intravaginal estriol once a week.
Drug Therapy for Stress Urinary Incontinence:
The first promising substance for pure SUI is duloxetine. Anticholinergic treatment is the first option if mixed stress incontinence with overactive bladder symptoms or overactive detrusor action is present.
Duloxetine:
Duloxetine is a serotonin and norepinephrine reuptake inhibitor (SSRI) on spinal level and reinforces the strength of the sphincter contraction. Duloxetine may reduce incontinence episodes by 50–60% (vs. 20–40% in the placebo group). For dosage and side effects, see the section "pharmacology of duloxetine". Duloxetine has been approved for the treatment of mild stress urinary incontinence in Europe. Duloxetine failed the US approval for stress urinary incontinence amidst concerns over liver toxicity and suicidal events.
Electromagnetic Stimulation of the Pelvic Floor Muscles:
Perineal nerves are stimulated by an electromagnetic chair, which leads to pelvic floor contraction. The treatment option is used for stress incontinence, overactive bladder, and mixed incontinence. Randomized trials could only demonstrate a small and temporary treatment effect with electromagnetic stimulation of the pelvic floor (Gilling et al., 2009) (Quek, 2005).
Surgical Treatment of Female Stress Urinary Incontinence
Periurethral Injections:
Collagen, Teflon, silicone, polydimethylsiloxane, or autologous fat are used for periurethral injections to improve sphincter function. In the long term, however, poor cure rates are reported (30–40%). If the periurethral injection is successful in the short term, the prognosis for a definitive cure with surgery (e.g., TVT, see below) is good.
Suprapubic and Abdominal Approach:
The Burch colposuspension has success rates of 70% in the long term. Any other (less invasive) treatment options have to compete with this success rate; unfortunately controlled trials are often not available. However, there is a significant decrease in abdominal procedures in favor of vaginal procedures.
Burch colposuspension:
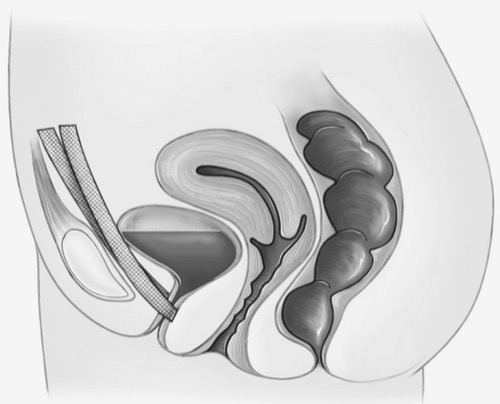
The paravaginal fascia is attached to the arcus tendineus ligament with mattress sutures which elevate the urethra and bladder neck. The Burch colposuspension can also be performed laparoscopically with fewer side effects, the success rate is somewhat lower (Dean et al., 2006).
Abdominal sacrocolpopexy:
Abdominal sacrocolpopexy is suitable to repair level 1 defects, treat the descensus of the uterus, and restore functional vaginal length and the vaginal axis. The vaginal cuff is mobilized and fixed to the os sacrum with a prolene mesh. The Y-shaped net extends into the anterior and posterior compartments, but the safety of these nets is controversial (see below). Surgery can be done with a laparoscopic or open approach.
Vaginal Approach for the Surgical Treatment of SUI:
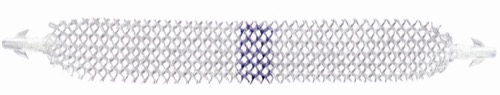
The vaginal approach with alloplastic meshes is most commonly used for surgical treatment of stress urinary incontinence, but the safety of these nets is controversial (see below).
Alloplastic Mid-urethral Slings:
All steps of the operation are done with the patient in a lithotomy position. A small incision of the anterior vaginal wall enables minimal dissection of the urethra. Two stab incisions for the urethral sling exit points are created suprapubic (TVT) or near the gracilis muscle origin (TOT). A 1 cm wide urethral sling is placed around the mid urethra using a special needle device and exiting at the two stab incisions. Wound healing and scarring lead to suburethral stability and restore pressure transmission. Details of the surgical techniques and complications are presented in the section alloplastic mid-urethral slings.
Suprapubic alloplastic mid-urethral slings have been first described as tension-free vaginal tape (TVT) (Ulmsten et al., 1998). TVT showed comparable 5-year results in randomized trials compared to the Burch colposuspension (Ward et al., 2006). Meanwhile, several medical companies with different sling materials and surgical techniques are present on the market [fig. alloplastic vaginal mid-urethral sling].
 |
Transobturator slings are known by the acronym TOT (transobturator tape). Randomized studies showed comparable results for TOT vs. TVT; however, long-term results are lacking (Latthe et al., 2010). As with suprapubic alloplastic mid-urethral slings, several medical companies with different sling materials and surgical techniques are present on the market [fig. Transobturator mid-urethral sling (TOT)]. Randomized trials showed comparable initial outcomes for TOT vs. TVT, but in the long term, the retropubic sling was advantageous regarding healing and urge symptoms (Alexandridis et al., 2023).
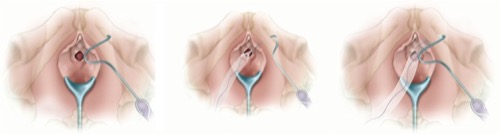 |
Minimally invasive alternatives to TVT or TOT are short mid-urethral devices (short tapes), which are inserted via a single vaginal incision and are anchored in the paraurethral tissue and pelvic floor muscles. Controlled trials with up to three years of follow-up showed comparable efficacy but trended toward higher rates of banding and revision surgery (Mostafa et al., 2014) (Abdel-Fattah et al., 2022).
 |
Pubovaginal Sling Procedure:
The pubovaginal sling procedure was only rarely performed after the development of the alloplastic mid-urethral slings. Now, the surgical technique is experiencing a certain renaissance due to the late complications of alloplastic material. A Pfannenstiel incision is used for a suprapubic approach, and autologous fascia material is harvested from the rectus sheath (1.5×10 cm). The urethra is exposed via a vaginal incision (comparable to TVT, see above). The fascia graft is passed on both sides from vaginal to suprapubic with the help of a Stamey needle and positioned like a TVT tape. The graft is fixed by tying the two ends of the sutures above the rectus sheath and with additional sutures to the paraurethral tissue. Compared to alloplastic slings, the pubovaginal sling procedure has somewhat poorer healing rates with regard to urinary incontinence, but complications from alloplastic material are avoided.
Vaginal surgery for pelvic floor insufficiency:
Procedures against urinary incontinence can be combined with pelvic floor reconstruction, see the section "pelvic floor insufficiency".
Risks by alloplastic mesh:
Complications such as chronic pain, dyspareunia up to 10%, mesh erosions (up to 12%), infections and the difficulty of removing the mesh in case of complications have led to warnings from several national supervisory authorities and led to the withdrawal of some products from the market. In some countries, the use of alloplastic mesh for the treatment of urinary incontinence and genital prolapse has been banned due to complications.
The current german guideline for the treatment of pelvic floor insufficiency, the SCENIHR recommendations of the EU and the EAU guidelines allow the use of alloplastic mesh materials in the pelvic floor area in certain risk constellations. However, a careful and more-thorough patient education about risks and alternatives is mandatory.
| SUI diagnosis | Index | Male SUI |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
V. Alexandridis, A. Lundmark Drca, M. Ek, and W. S. derberg, “Retropubic slings are more efficient than transobturator at 10-year follow-up: a Swedish register-based study.,” Int Urogynecol J., vol. 34, no. 6, pp. 1307–1315, 2023.
A. Mostafa, C. P. Lim, L. Hopper, P. Madhuvrata, and M. Abdel-Fattah, “Single-incision mini-slings versus standard mid-urethral slings in surgical management of female stress urinary incontinence: an updated systematic review and meta-analysis of effectiveness and complications.,” Eur Urol, vol. 65, no. 2, pp. 402–427, 2014.
Dean, N. M.; Ellis, G.; Wilson, P. D. & Herbison, G. P.
Laparoscopic
colposuspension for urinary incontinence in women.
Cochrane
Database Syst Rev, 2006, 3, CD002239
Gilling, P. J.; Wilson, L. C.; Westenberg, A. M.;
McAllister, W. J.; Kennett, K. M.; Frampton, C. M.; Bell, D. F.; Wrigley,
P. M. & Fraundorfer, M. R.
A double-blind randomized controlled
trial of electromagnetic stimulation of the pelvic floor vs sham therapy
in the treatment of women with stress urinary incontinence.
BJU
Int, 2009, 103, 1386-1390
Latthe, P. M.; Singh, P.; Foon, R. & Toozs-Hobson, P.
Two
routes of transobturator tape procedures in stress urinary incontinence: a
meta-analysis with direct and indirect comparison of randomized trials.
BJU
Int, 2010, 106, 68-76
Liedl u.a. 2005 LIEDL, B. ; SCHORSCH, I. ;
STIEF, C.:
[The development of concepts of female (in)continence.
Pathophysiology, diagnostics and surgical therapy].
In: Urologe A
44 (2005), Nr. 7, S. W803–18; quiz W819–20
Mariappan, P.; Alhasso, A.; Ballantyne, Z.; Grant, A. &
N'Dow, J.
Duloxetine, a serotonin and noradrenaline reuptake inhibitor
(SNRI) for the treatment of stress urinary incontinence: a systematic
review.
Eur Urol, 2007, 51, 67-74.
Quek, P.
A critical review on magnetic stimulation:
what is its role in the management of pelvic floor disorders?
Curr
Opin Urol, 2005, 15, 231-235
Ward, K. L.; Hilton, P.; K., U. & Group, I. T. T.
Tension-free
vaginal tape versus colposuspension for primary urodynamic stress
incontinence: 5-year follow up.
BJOG, 2008, 115,
226-233
Viktrup u.a. 2004 VIKTRUP, L. ; SUMMERS,
K. H. ; DENNETT, S. L.:
Clinical practice guidelines for the initial management of urinary
incontinence in women: a European-focused review.
In: BJU Int
94 Suppl 1 (2004), S. 14–22
 Deutsche Version: Belastungsinkontinenz der Frau
Deutsche Version: Belastungsinkontinenz der Frau
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.