You are here: Urology Textbook > Surgery (procedures) > Simple suprapubic prostatectomy
Suprapubic Simple Prostatectomy: Surgical Technique and Complications
Indications for Suprapubic Simple Prostatectomy
Surgical treatment of benign prostatic hyperplasia is necessary in cases of recurrent urinary retention, recurrent urinary tract infections, recurrent hematuria, bladder stones, postrenal kidney failure, and large bladder diverticula. The most common indication for surgical therapy is moderate to severe symptoms of BPH, which are inadequately relieved with medication and limit the patient's quality of life.
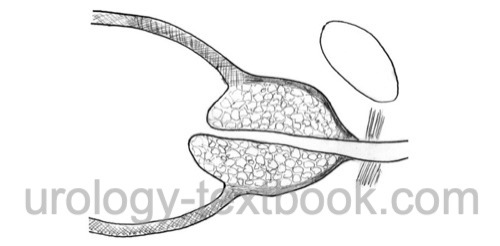
The surgical technique of transvesical simple prostatectomy [fig. principle of suprapubic prostatectomy] is indicated for very large adenoma (>75 ml) or contraindications for lithotomy position. The transvesical approach enables treatment of bladder diverticula or bladder stones at the same time. Inguinal hernia may be treated simultaneously with an adenomectomy.
Contraindications to Suprapubic Prostatectomy
Prostate cancer, low life expectancy, coagulation disorders, and untreated urinary tract infection.
Surgical Technique of Suprapubic Simple Prostatectomy
Preoperative Patient Preparation
- Exclude or treat urinary tract infections
- Perioperative antibiotic prophylaxis
- General anesthesia or spinal anesthesia
- Supine position with slight hyperextension of the lumbar spine
- Disinfection and draping
- Fill the bladder with 200–300 ml saline.
Surgical Approach:
- Lower midline incision or Pfannenstiel incision
- Cut the linea alba.
- After blunt dissection of the retropubic space, insert a wound retractor.
- Vertical cystostomy, which is secured with sutures to prevent further tearing.
- Remove bladder stones or resect bladder diverticula if present.
Dissection of the Prostatic Adenoma:
- Circular incision of the bladder neck with the electric scalpel after identification of the ureteral orifices
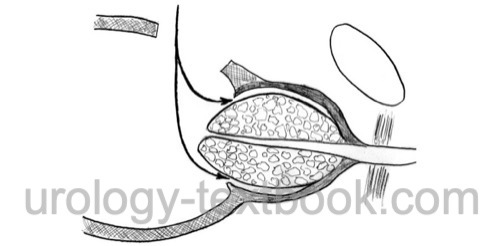
- Develop the plane between prostatic adenoma and peripheral prostatic tissue ("prostatic capsule") with scissor dissection.
- Blunt finger dissection completes the mobilization of the prostatic adenoma. The apical dissection should avoid excessive traction of the urethra (and the urinary sphincter).
 |
 |
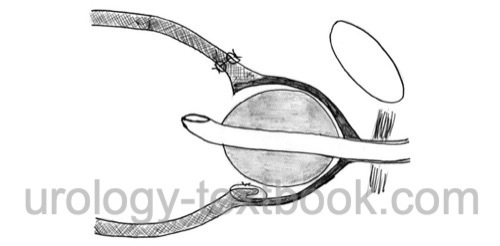 |
Hemostasis after Suprapubic Prostatectomy:
- The bladder mucosa is readvanced into the prostatic fossa by two figure-of-eight sutures at the 4 and 8 o'clock positions (do not incorporate the ureteric orifices).
- A running suture of the bladder neck is done between the figure-of-eight sutures.
- The described sutures should stop major bleeding; control further bleeding with electrocautery or additional suture ligatures.
- Place an irrigation catheter (20–22 CH) into the bladder with balloon inflation in the prostatic fossa (50–100 ml, depending on the size of the prostatic adenoma).
- If hemostasis is insufficient after blocking the catheter, narrow the bladder neck to tamponade the prostatic fossa with fast absorbable sutures (purse-string suture). The bladder neck can be opened after 8 days using the catheter balloon, or the spontaneous resolution of the sutures has to be awaited.
Wound Closure:
- Optional: insert a suprapubic tube
- Two-layer closure of the cystotomy
- Irrigate the wound cavity
- Insert a wound drainage (e.g., closed gravity system)
- Separate closure of fascia, subcutis, and cutis
Postoperative Management after Suprapubic Prostatectomy
General measures: consider patient-controlled analgesia for pain management. Early mobilization and exercises to prevent thrombosis and pneumonia. Thrombosis prophylaxis. Laboratory tests (hemoglobin, creatinine), regular physical examination of the abdomen, and incision wound.
- After surgery: continuous irrigation of the bladder. Control excessive bleeding by increasing the catheter blockage or by gentle traction on the catheter. If not successful, proceed with transurethral coagulation to control bleeding.
- First day: reduce or stop the continuous irrigation. Patient ambulation.
- Second day: deflate the catheter balloon to 30 ml. Remove the wound drainage (if <75 ml/24 h drainage).
- Third to fifth day: remove the irrigation catheter; consider cystography to ensure a watertight bladder closure
Complications of Suprapubic Prostatectomy
- Often retrograde ejaculation (80–90%)
- Bleeding: re-exploration (transurethral coagulation, evacuation of bladder tamponade) and blood transfusion are possible.
- Initial urinary incontinence is often due to an overactive bladder. Rarely persistent urinary incontinence due to urinary sphincter damage.
- Rarely persistent Erectile dysfunction
- Urinary tract infections
- Ureteral injury.
- Bladder neck sclerosis, urethral stricture
- Surgical site infections
- Urinoma
- Thrombosis, pulmonary embolism
| Greenlight laser vaporization of the prostate | Index | Retropubic simple prostatectomy |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
J. A. Smith, S. S. Howards, G. M. Preminger, and R. R. Dmochowski, Hinman’s Atlas of Urologic Surgery Revised Reprint. Elsevier, 2019.
 Deutsche Version: transvesikale Adenomektomie
Deutsche Version: transvesikale Adenomektomie
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.