You are here: Urology Textbook > Urologic examinations > Blood tests > Testosterone
Testosterone in Serum – Lab Test
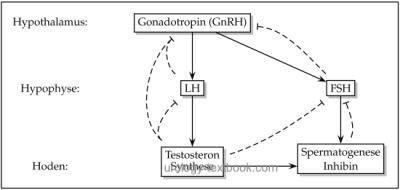
Testosterone is the most important male sex hormone. The hypothalamic-pituitary-gonadal hormone axis controls the release of testosterone [fig. control of testosterone]. 60% of the testosterone is bound to the sex hormone binding globulin (SHBG), due to the strong bound it is considered biological inactive. Only 1–3% of total testosterone are unbound in plasma (free testosterone). The remaining portion is albumin bound, which is considered to be weak bound. Free testosterone and albumin-bound testosterone are called bioavailable testosterone, because both can exert biological activity.
 |
Standard Value:
Depending on age 12–35 nmol/l (3,5–10 ng/ml) in the morning. The testosterone circadian rhythm peaks early in the morning, concentrations are 40% lower in the evening (Trottmann, 2010).
Standard Value of Free Testosterone:
>0,25 nmol/l (>7,2 ng/dl).
Laboratory test method:
Competitive immunoassay for the testosterone concentration. Free testosterone is calculated with the Vermeulen formula using testosterone, SHBG and albumine (Vermeuten et al., 1999).
Indications:
The testosterone concentration is an important diagnostic parameter in andrological diseases. Further indications are the control of antiandrogenic therapy by GnRH analogs in prostate cancer and the evaluation of hormone status in patients with a testicular tumor. LH, FSH and SHGB are determined in case of abnormalities of testosterone. Free testosterone is helpful to assess inconclusive low concentrations of testosterone.
Confounders:
Elevated levels are seen due to anticonvulsants, barbiturates, clomiphene, estrogens or oral contraceptives. Low levels are caused by androgen medication (or abuse), cyproterone, GnRH analogs, GnRH antagonists, digitalis, glucocorticoids, halothane, ketoconazole, metoprolol, phenothiazines, spironolactone and tetracyclines.
Differential Diagnosis of Hypogonadism
Hypogonadism is an endocrine dysfunction of the testes with testosterone deficiency. Primary hypogonadism is caused by a failure of the testosterone production in the testes, the releasing hormones are compensatorily increased (hypergonadotropic hypogonadism). Secondary hypogonadism is caused by a defect of the pituitary hormone release (hypogonadotropic hypogonadism). Tertiary hypogonadism is caused by a defect of the hypothalamus (Koehn, 2004). For more details please see also section testosterone deficiency.Differential Diagnosis of Hypergonadism
Hypogonadotropic hypergonadism is more common in men: testosterone abuse, increased SHBG, hormone-active testicular tumors (e.g., Leydig cell tumor) or adrenal tumors. Hypergonadotropic hypergynadism is seen in the androgen insensitivity syndrome.
| PT | Index | SHBG |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Guder, W. G. & Nolte, J. Das Laborbuch für Klinik und PraxisUrban + Fischer, 2009
Köhn, F.-M. (2004). [diagnosis and therapy of hypogonadism in adult males].
Urologe A, 43(12):1563-81; quiz 1582–3.
Trottmann, M., Dickmann, M., Stief, C. G., and Becker, A. J. (2010).
[laboratory workup of testosterone].
Urologe A, 49(1):11–15.
Siegenthaler 1988 SIEGENTHALER, W. ;
SIEGENTHALER, W. (Hrsg.):
Differentialdiagnose innerer Krankheiten.
Georg Thieme Verlag, Stuttgart, New York., 1988
Vermeulen, A.; Verdonck, L. & Kaufman, J. M.
A critical evaluation of simple methods for the estimation of free
testosterone in serum.
The Journal of clinical endocrinology and
metabolism, 1999, 84, 3666-3672
 Deutsche Version: Testosteronspiegel
Deutsche Version: Testosteronspiegel