You are here: Urology Textbook > Surgery (procedures) > Transureteroureterostomy
Transureteroureterostomy: Surgical Technique and Complications
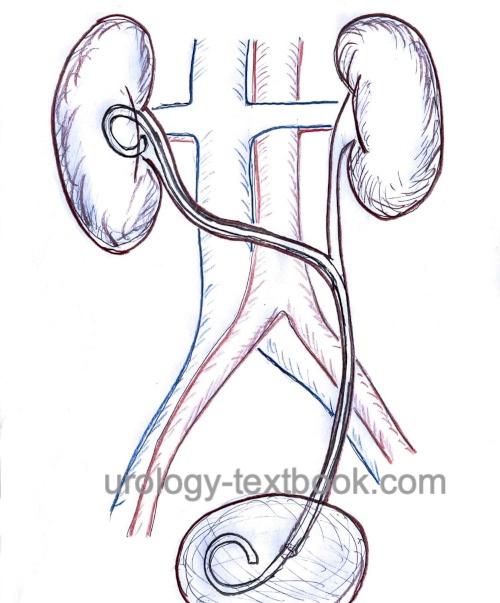
Transureteroureterostomy is used to bypass a diseased distal ureter with an end-to-side anastomosis of the donor (diseased) ureter with the recipient (healthy) ureter on the opposite side. Transureteroureterostomy is rarely used for the following indications (Barry, 2005):
Indication for Transureteroureterostomy
- Injury or defects of the distal ureter if a psoas hitch or Boari flap is not possible (e.g., previous surgery or radiotherapy in the small pelvis)
- Urinary diversion with ureterocutaneostomy
 |
Contraindications
- Coagulation disorders.
- Long ureteral stricture or ureteral defects not allowing a tension-free end-to-end anastomosis.
- Kidneys without sufficient function (<15% of total glomerular filtration rate)
- Further contraindications depend on the surgical risk due to the comorbidity of the patient, the renal function of the contralateral kidney, and the surgical procedure's impact on the patient's quality of life.
- Be cautious concerning diseases with a high risk of recurrence and danger to distal ureteral function: radiotherapy near the ureters, recurrent nephrolithiasis, urothelial carcinoma, diseases of the aorta, retroperitoneal fibrosis, and pelvic tumors.
Surgical Technique of Transureteroureterostomy
Preoperative Patient Preparation
- Exclude or treat urinary tract infection
- Perioperative antibiotic prophylaxis
- Retrograde pyelography to confirm the diagnosis and length of the ureteral defect.
- Transurethral catheter
Surgical Approach
Median laparotomy is the standard approach, incise the white line of Toldt on both sides and identify both ureters. Depending on the underlying disease, mobilize and resect the distal ureter on the diseased side. Carefully mobilize the proximal end of the diseased ureter with attention to the vascular supply. Dilate a tunnel from the left to the right retroperitoneum with finger dissection under the mesentery and above the large vessels. Alternatively, incise the posterior peritoneum and mobilize the bowel's meso comparable to retroperitoneal lymphadenectomy. Guide the diseased proximal ureter to the opposite side without kinking.
Transureteroureterostomy:
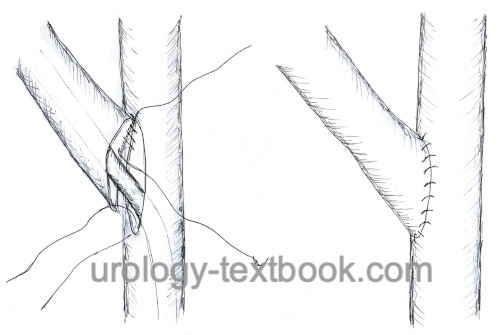
- Spatulate the diseased ureter over 3cm.
- The healthy ureter is only minimally mobilized and opened over 3cm medially longitudinally in the area of the planned anastomosis using vascular scissors.
- Advance a DJ ureteral stent into the urinary bladder via the ureterotomy of the healthy ureter; the other end is advanced into the contralateral kidney via the diseased ureter.
- Place corner sutures (PDS 5-0); suture the posterior wall of the anastomosis in a running fashion from the inside and the anterior wall of the anastomosis from the outside.
- Insert a wound drainage near the ureteral anastomosis.
- Wound closure
 |
Postoperative Care after Transureteroureterostomy
General measures:
Early mobilization, thrombosis prophylaxis, respiratory therapy, laboratory tests (hemoglobin, creatinine), regular physical examination of the abdomen and incision wound.
Analgesia:
Analgesics with a combination of NSAIDs and opioids. Peridural anesthesia facilitates postoperative pain management.
Drains and catheters:
Remove the retroperitoneal drainage if the daily drainage is below 50 ml. The bladder catheter stays additional 1–2 days or 3–5 days in total, and the ureteral stent for 2–4 weeks.
Complications of Transureteroureterostomy
Bleeding, infection, urinoma, recurrent ureteral stricture, loss of kidney function, injury to adjacent organs (bowel, liver, spleen, pancreas).
| Urologic Surgery | Index | Ureterocystoneostomy for VUR |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
J. M. Barry, “Surgical atlas transureteroureterostomy.,” BJU Int., vol. 96, no. 1, pp. 195–201, 2005, doi: 10.1111/j.1464-410X.2005.05552.x.
 Deutsche Version: Transureteroureterostomie
Deutsche Version: Transureteroureterostomie