You are here: Urology Textbook > Surgery (procedures) > TURB
Transurethral Resection of the Bladder (TURB): Technique and Complications
Indications for transurethral resection of the bladder (TURB)
- Diagnosis (Biopsy) of bladder tumors
- Endoscopic curative treatment of superficial bladder cancer
- Palliative therapy of advanced bladder tumors
- Rare: diagnosis and therapy of interstitial cystitis
 |
 |
Surgical Technique of Transurethral Bladder Resection
Preoperative patient preparation:
Urinary tract infection excluded or treated, Perioperative antibiotic prophylaxis, lithotomy position.
Anesthesia:
Spinal anesthesia or general anesthesia is needed for TURB. Spinal anesthesia offers theoretical advantages for the initial postoperative period: the patient is calm without pressing or coughing, and the manipulation of the catheter is possible without pain. General anesthesia with muscle relaxation eliminates the risk of an obturator reflex (see complications) and is preferable for lateral tumors.
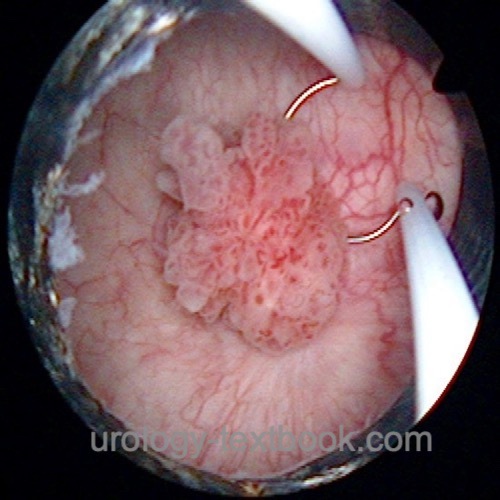
Cystoscopy:
Check for the width of the urethra, and search for urethral tumors. The mucosa of the bladder (and prostate) is examined to identify all flat and papillary tumors. Document the size, number, localization, and appearance of all visible lesions before TURB.
Fluorescence cystoscopy:
Fluorescence cystoscopy with blue light after prior instillation of hexaminolevulinate (Hexvix) results in better detection of urinary bladder carcinoma with a 20% higher tumor detection rate and 40% improved detection of CIS (Jocham et al., 2005).
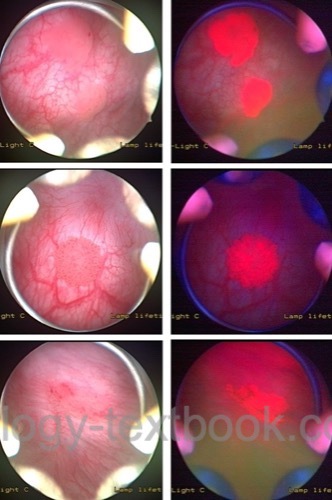 |
Indications:
High-grade cells in urine cytology, all patients with a history of multifocal or high-grade carcinoma.
Technique:
Instillate hexaminolevulinate (Hexvix) into the bladder one hour before TURB. Perform cystoscopy with white and blue light, resect (TURB) all abnormal lesions under both examination conditions.
Contraindications:
Intravesical therapy or TURB in the last 6–10 weeks, urinary tract infection, women of childbearing age.
Standard TURB
- A resectoscope is introduced into the bladder (around 24 CH). If the meatus is too narrow, dilatation may be necessary. Urethral strictures need to be treated with internal urethrotomy.
- Visible tumor vessels are coagulated at the base of the tumor.
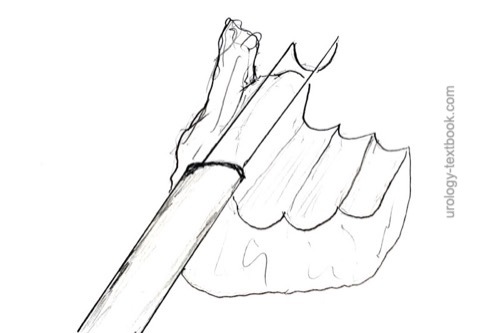
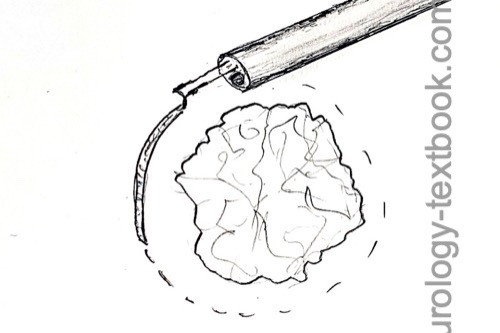
- The bladder tumor is resected with the resection loop [fig standard TURB 1 and standard TURB 2]; this results in a fragmented tumor specimen. After the complete resection of the bladder tumor, the specimen is collected with a bladder syringe.
- A separate specimen of the tumor margin and base is collected to check for complete resection and to facilitate the identification of muscle-invasive bladder cancer.
- Multiple small lesions, especially in known bladder cancer, are treated with fulguration.
- Meticulous hemostasis finishes the operation, an irrigation catheter is introduced (18–22 CH, depending on bleeding and resection size).
 |
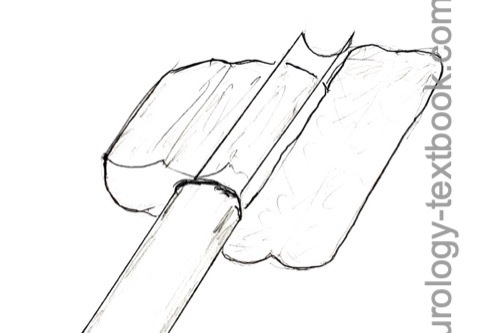 |
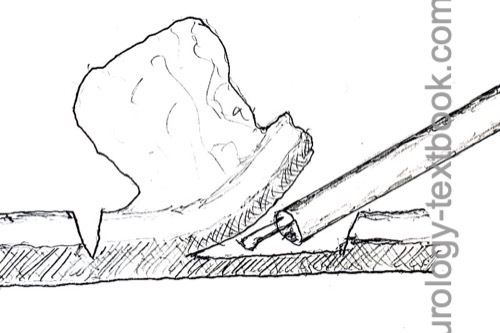
En-block resection:
En-block resection is a good option for smaller tumors under 3 cm in size. Advantages are better detection of infiltration depth by the pathologist and less tumor cell seeding in the urinary bladder. The retrieval of larger tumors through the urethra is problematic. The first step is circular coagulation of the tumor base, followed by a circular incision into the tunica muscularis with the resection loop. With careful application of electrocautery, the tumor base is dissected out of the muscularis while pushing or pulling with the resection loop. Laser techniques and using a waterjet scalpel for dissection in the bladder wall are also reported (Kramer et al., 2012).
 |
 |
Postoperative Care after TURB
Early instillation of Mitomycin C:
- The early instillation of mitomycin C reduces the risk of bladder tumor recurrence by 50%.
- Dosage: instillation of 40 mg mitomycin C in 40 ml normal saline into the bladder for one hour. The instillation is best done immediately after surgery.
- Contraindications: perforation of the bladder, severe postoperative bleeding.
General measures:
Early mobilization, thrombosis prophylaxis only for patients with risk factors, pain medication, and antimuscarinic agents against catheter-related discomfort.
Irrigation catheter:
Irrigation prevents clot formation and may reduce the risk of tumor recurrence. Remove the catheter after 1–3 days, depending on the resection depth and postoperative bleeding.
Complications of transurethral resection of the bladder (TURB)
- Bladder perforation (2–10%): is managed with catheter drainage for 4–7 days, depending on the size and depth of the perforation. Healing can be controlled with cystography. Surgical exploration and repair are rarely needed.
- Severe bladder perforation can happen with obturator nerve stimulation during the resection of lateral tumors. Obturator nerve reflexes may require general anesthesia with muscle relaxation or an obturator nerve block. Spinal anesthesia does not prevent obturator nerve reflexes.
- Bleeding, clot retention, bladder tamponade. Transurethral tamponade evacuation (and coagulation) with general anesthesia is necessary for up to 3%.
- Infection
- Urethral injury and urethral stricture formation
- Vesicoureteral reflux, ureteral injury or obstructive uropathy, if resection across the ureteral orifice was necessary (Collado et al., 2000).
| Endoscopic or transurethral cystolitholapaxy | Index | Mid-urethral slings |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Collado, A.; Chechile, G. E.; Salvador, J. & Vicente, J.
Early complications of endoscopic treatment for superficial bladder tumors
J Urol, 2000, 164, 1529-32
 Deutsche Version: Transurethrale Resektion der Harnblase (TURB)
Deutsche Version: Transurethrale Resektion der Harnblase (TURB)
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.