You are here: Urology Textbook > Surgery (procedures) > Ureteral reimplantation
Ureteral Reimplantation: Psoas Hitch and Boari-Flap Techniques
Ureterocystoneostomy is the reimplantation of the ureter into the urinary bladder; distal and mid-ureteral defects can be bridged (combined with using bladder tissue) in the case of:
Contraindications
- Coagulation disorders.
- Long ureteral stricture or injuries, which do not allow a tension-free end-to-end anastomosis.
- Kidneys without sufficient function (<15% of total glomerular filtration rate)
- High surgical risk due to the comorbidity of the patient.
- Insufficient bladder capacity.
Surgical Technique of Ureteral Reimplantation to Bridge Ureteral Defects
Preoperative Patient Preparation
- Cystoscopy, retrograde pyelography and ureteroscopy to confirm the diagnosis, try to insert a DJ ureteral stent.
- Exclude or treat urinary tract infections
- Perioperative antibiotic prophylaxis
- Transurethral bladder catheter after disinfection and sterile draping.
Surgical Approach
Suitable surgical approaches depend on the indication and previous surgery: lower midline incision, gibson incision or paramedian laparotomy are possible. First steps are the extraperitoneal mobilization of the bladder. As far as possible, the peritoneum is dissected of the bladder. Depending on previous operations, a transperitoneal approach is more realistic. The ureter is marked with a vessel loop after identification. Depending on the underlying disease, ligate the distal diseased ureter or choose distal ureteral resection. The proximal end of the diseased ureter should be without scar tissue; spatulate the end and insert a ureteral stent (MJ) fixed with a rapidly absorbable suture. Pay attention to the ureteral vascular supply during all steps.
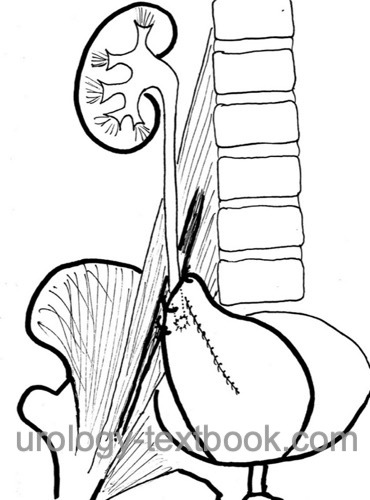
Psoas Hitch Ureteral Reimplantation:
The Psoas Hitch technique can bridge up to 10 cm of defective ureter.
- The opened urinary bladder is shifted in the direction of the kidney with the help of loose fixation sutures on the psoas muscle. Watch out for the genitofemoral nerve!
- You get maximun mobilization of the bladder to the retroperitoneum if you open the bladder transversely to the shifting and close lengthwise after reimplantation.
- Create a neo-hiatus above the fixation sutures, and reimplantant the ureter using the technique of Leadbetter-Politano or direct anastomosis without antireflux technique.
 |
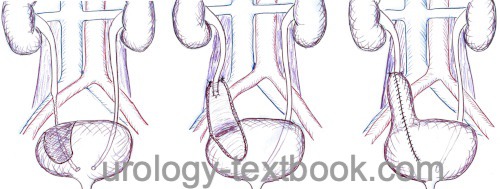
Boari Flap Ureteral Reimplantation:
The Boari flap technique can bridge up to 15 cm of defective ureter (depending on the capacity of the urinary bladder).
- A bladder flap is raised towards the kidney. The flap should be at least 4 cm wide at the base. The length-to-width ratio of the flap should be a maximum of 3:1 to avoid ischemia in the implantation area.
- Attach the flap to the psoas muscle with fixation sutures (Cave: genitofemoral nerve).
- Reimplantant the ureter using the technique of Leadbetter-Politano or direct anastomosis without antireflux technique.
- Close the bladder flap in a tubular fashion.
 |
Drainage:
Insert a drain near the anastomosis. Exit the ureteral stent through a separate stab incision of bladder and skin.
Technical Modifications:
The Psoas hitch and the Boari flap procedure can be performed laparoscopically (robotic-assisted) in experienced hands.
Postoperative Care after Ureteral Reimplantation
General measures:
Early mobilization, thrombosis prophylaxis depending on age, laboratory tests (hemoglobin, creatinine), regular physical examination of the abdomen and incision wound.
Analgesia:
Analgesics with a combination of NSAIDs and opioids.
Drains and Catheters:
Remove the pelvic drain if the daily drainage volume is below 50 ml, ureteral splint after 5–7 days, and bladder catheter after 5–10 days. Removal (consider cystography) depends on the amount of bladder reconstruction.
Complications of Ureteral Reimplantation
- Reduced bladder capacity: Pollakiuria, nocturia, urge symptoms, and urge incontinence.
- Hydronephrosis: postoperative hydronephrosis often improves spontaneously after resolution of the postoperative edema and hematoma. Ureteral stricture may result from scarring, kinking of the ureter, or ischemia, forcing ureteral stenting and surgical revision.
- Further complications: vesicoureteral reflux, hemorrhage, wound infection, urinary tract infections, urinoma. Injury to neighboring organs (bowel, nerves, vas deferens).
| Ureterocystoneostomy for VUR | Index | Megaureter surgery |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Hinman: Atlas Urologischer Operationen im Kindes- und Erwachsenenalter.
 Deutsche Version: Harnleiterreimplantation: Technik nach Leadbetter, Lich-Gregoir, Psoas hitch und Boari Lappen
Deutsche Version: Harnleiterreimplantation: Technik nach Leadbetter, Lich-Gregoir, Psoas hitch und Boari Lappen