You are here: Urology Textbook > Surgery (procedures) > Ureteroscopy
Ureteroscopy: Ureteroscopy: Surgical Steps and Complications
Indications for Ureteroscopy
- Abnormal imaging findings (obstruction, ureteral strictures, filling defects)
- Diagnosis of hematuria
- Diagnosis of pathologic urine cytology
- Diagnosis and treatment of ureteral stones and kidney stones
- Diagnosis or treatment of ureteral strictures
- Diagnosis and treatment of upper tract urothelial cancer
 |
Contraindications to Ureteroscopy
Urinary tract infection, urosepsis. Relative contraindications are coagulation disorders, pregnancy, or contraindications for lithotomy position.
Equipment for Ureteroscopy
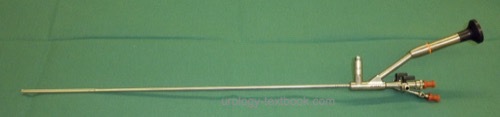
Semirigid ureteroscopes look like long, thin cystoscopes They usually have non-interchangeable lenses with a 0–10 degree angle of view. The working channel is 5 CH wide, and there is a connection for irrigation inflow and outflow. The thickness of a semirigid ureteroscope is between 6–9 CH, thin at the tip, with a gradual increase in diameter. Technical refinements have enabled semirigid ureteroscopes with 5–7 CH in diameter and two separate working channels.
Flexible ureteroscopes are 8–10 CH in diameter, and the working channel is thinner (CH 3). Modern flexible ureteroscopes have an additional channel for irrigation. The tip can be actively controlled with deflection up to 270 degrees [fig flexible ureteroscopy]. Modern devices do not use fiber optics; a camera chip on the tip (CCD sensor) provides a high-resolution image of high quality.
 |
Technique of Ureteroscopy
Preoperative Patient Preparation
- Exclude or treat urinary tract infection
- General anesthesia or spinal anesthesia is necessary
- Perioperative antibiotic prophylaxis
- Lithotomie position
Cystoscopy and Retrograde Pyelography
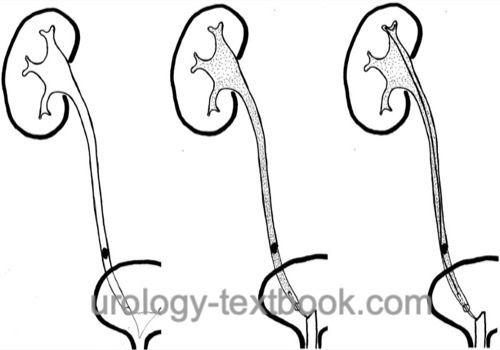
After cystoscopy, retrograde pyelography is performed to evaluate the anatomy of the upper urinary tract and the indications for ureteroscopy. A guide wire is inserted up to the renal pelvis with the ureteral catheter [fig. retrograde pyelography].
 |
Semirigid Ureteroscopy
A narrow ostium makes the dilatation of the prevesical ureter necessary [fig. dilatation of the distal ureter (left picture)]. Alternatively, the urinary tract is dilated with DJ stents and the ureteroscopy is postponed for 2–4 weeks.
The ureteroscope is advanced along the urethra and guide wire, until the ostium is in sight. If the intubation of the orifice is technically difficult, a second guide wire or thin ureteral catheter may help [fig. entry of the distal ureter with the ureteroscope].
 |
The ureteroscope is advanced along the guide wire under direct vision into the ureter. The irrigation should be adjusted as low as possible. A kinking of the ureter can be straightened with the help of guide wires and ureteral catheters [fig. straightening a ureteral kinking during ureteroscopy].
 |
Flexible Ureteroscopy
After inserting the guide wire, an access sheath is inserted into the proximal ureter for easy repeated entry of the flexible ureteroscope, especially when a significant stone burden is encountered. After advancing the flexible ureteroscope into the renal pelvis, every renal calyx is inspected [fig. flexible ureteroscopy].
Ureteroscopic Treatment of Urolithiasis
Extraction of ureteral stones with grasping forceps:
Small ureteral stones can be easily extracted with grasping forceps. Forceps for ureteroscopy are mostly reusable; their application is cheap.
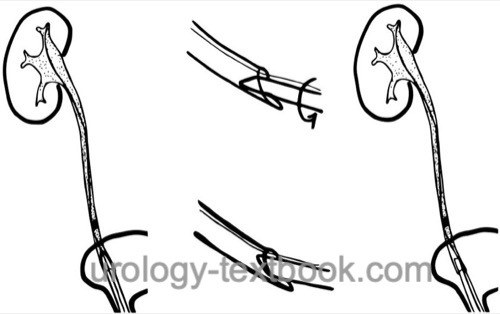
Extraction of ureteral stones with Dormia baskets:
Ureteral stones that are small enough to be extracted completely can easily be removed with Dormia baskets [fig. extraction of ureteral stone with Dormia basket]. The major disadvantage of Dormia baskets is the cost of the disposable instrument.
First, the closed Dormia basket is advanced between the stone and the ureter wall. Beware of fixed ureteral stones; it is easy to perforate the fragile ureteral wall. Above the stone, the stone basket is opened and pulled back. The ureteral stone is manipulated (e.g., rotating) into the center of the basket. The stone basket is slowly closed until the stone is trapped within the basket. Slowly withdraw the ureteroscope with the basket and control the stone movement with direct vision. The ureteral stone should glide along the urothelium. If the extraction with the stone basket is not possible due to size, proceed with lithotripsy of the stone (see below).
Lithotripsy of ureteral stones:
Larger ureteral stones cannot be extracted in toto, a lithotripsy in the ureter is necessary. Afterward, the fragments can be removed. The following possibilities for ureteroscopic lithotripsy exist:
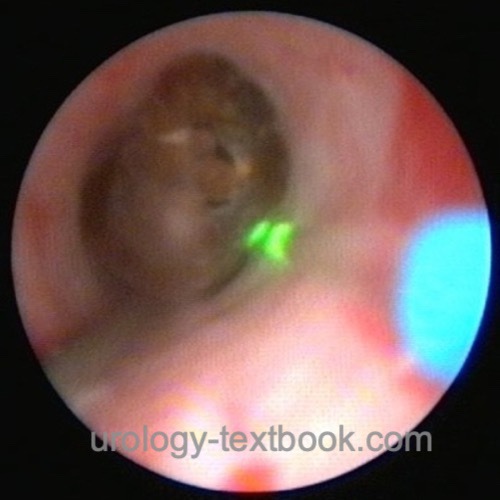
- Laser lithotripsy (e.g., Holmium)
- Electromechanical lithotripsy (e.g., Lithoclast)
- Electrohydraulic lithotripsy (EHL)
Laser lithotripsy has several advantages: effective lithotripsy with different settings, minimized trauma to the ureter, and reduced stone dislocation during lithotripsy [fig. Holmium-Laser lithotripsy]. Furthermore, thin 3 CH-probes for flexible ureteroscopy are available. Depending on the energy source and settings, lithotripsy may produce small stone fragments, which are removed afterward with a stone basket, or the ureteral stone is pulverized (stone dusting).
 |
Ureteroscopic Treatment Options for Strictures and Tumors
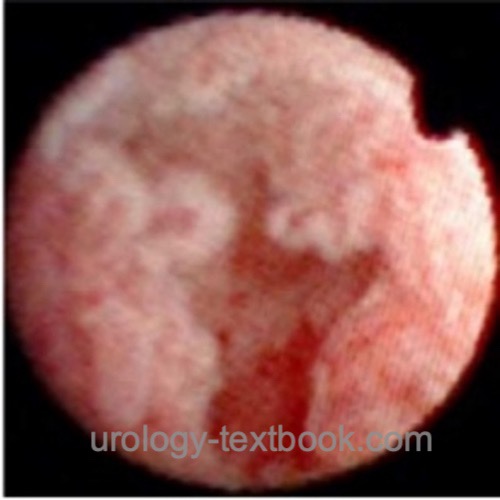
Ureteroscopic biopsy:
Biopsies should be taken from tumors or strictures of unknown etiology. For rigid or flexible ureteroscopes, there exist a varitey of biopsy forceps. The amount of resulting tissue with ureteroscopic biopsy is very small. Multiple biopsies are necessary, to obtain a reliable diagnosis. Tissue sampling of papillary tumors is also successful using a Dormia basket.
Ablation of ureteral tumors:
Endoscopic palliative treatment of ureter or renal pelvis tumors is possible with ureteroscopic resectoscopes. Alternatively, tumor ablation is possible using laser coagulation.
Ureteroscopic incision of ureteral strictures:
See section ureteral strictures.
Stenting of the Ureter
After ureteroscopy, especially after more extended manipulation, a DJ ureteral stent is necessary for 2–4 weeks. After perforation of the ureter, a bladder catheter (for a few days) and a DJ ureteral stent should be placed to allow pressure-free urine drainage. The placement of a DJ has been dispensed with success (in several randomized trials) after uncomplicated ureteroscopy (e.g., after ureteral stone extraction).
Atlas of Ureteroscopy Findings
 |
 |
 |
 |
 |
 |
 |
 |
 |
Complications of Ureteroscopy
- Postoperative hydronephrosis and flank pain due to wall edema, blood clots, residual stones, or ureteral injury.
- Complications of the DJ ureteral stent: pain, LUTS, dislocation, forgotten stent removal with stone formation.
- Febrile urinary tract infection, urosepsis (1–3%)
- Bleeding, clot retention, perirenal hematoma.
- Ureteral injuries: perforation (2–10%), urinoma, ureteral stricture (1–3%), ureteral avulsion (0.1–0.2%).
| ESWL | Index | Open nephroureterectomy |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
De Coninck V, Keller EX, Somani B, Giusti G, Proietti S, Rodriguez-Socarras M, Rodríguez-Monsalve M, Doizi S, Ventimiglia E, Traxer O. Complications of ureteroscopy: a complete overview. World J Urol. 2020 Sep;38(9):2147-2166. doi: 10.1007/s00345-019-03012-1.
 Deutsche Version: Harnleiterspiegelung
Deutsche Version: Harnleiterspiegelung