You are here: Urology Textbook > Bladder > Vesicovaginal fistula
Vesicovaginal Fistula: Etiology, Diagnosis, and Treatment
Definition
A vesicovaginal fistula is an abnormal passageway between the female urinary bladder and vagina with urinary incontinence.
Etiology of Vesicovaginal Fistula
- Hysterectomy (in 0.1–2%, depending on the indication for surgery)
- Gynecological tumors: infiltration, radiation therapy or surgical treatment.
- Prolonged obstructed labor with pressure necrosis of the anterior vaginal wall and the bladder neck (this is the most common cause of a vesicovaginal fistula in developing countries).
- Obstetric surgery
- Trauma
Signs and Symptoms
Urinary incontinence (continuously day and night), loss of urine through the vagina, urinary tract infections.
Diagnostic Workup
- Pelvic examination: after indigo carmine injection into the urinary bladder, an inserted vaginal swab turns blue.
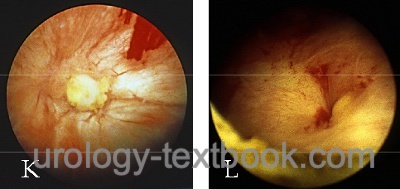
- Cystoscopy with biopsy and possibly retrograde pyelography to rule out ureteral injury.
- VCUG: to diagnose and locate the fistula.
- Abdominal CT scan to rule out ureteral injury and to search for pelvic tumors.
 |
Treatment of Vesicovaginal Fistula
Conservative Treatment:
A newly diagnosed vesicovaginal fistula after gynecological surgery may be cured by inserting an indwelling catheter for 3–4 weeks (success rate 10–50%). The success is difficult to predict in individual cases; indicators of a good prognosis are early diagnosis and therapy within seven days, small fistulas of less than 1 cm in size, no loss of urine after inserting the bladder catheter, and no previous radiation treatment or cancer surgery.
Timing of Surgical Treatment:
The time delay between fistula formation and surgical treatment is stressful for the patient. Uncomplicated fistula after pelvic surgery may be treated without delay. Fistula repair caused by prolonged obstructed labor should be delayed for three months to allow healing of the inflammatory and necrotic tissue reaction around the fistula. Vaginal estrogen application is recommended before surgery for postmenopausal women. Some authors recommend a delay of up to one year before repair of radiation therapy induced fistulas.
Vaginal Approach for the Repair of Vesicovaginal Fistulas:
Vaginal surgical techniques are possible for uncomplicated and small vesicovaginal fistulas. The main advantage of the vaginal approach is the low postoperative morbidity.
Surgical technique of the vaginal approach:
- Circular incision around the fistula tract and mobilization of the anterior vaginal wall.
- Two layer closure of the bladder wall (urothelium and tunica muscularis).
- Mobilize a peritoneal or Martius flap (adipose tissue from the labia majora) to cover the sutured bladder lesion.
- Closure of the anterior vaginal wall.
- Transurethral catheter for bladder drainage. Check vesical integrity after two weeks with cystography and remove the catheter.
Abdominal Approach for the Repair of Vesicovaginal Fistulas:
The abdominal approach is more risky for the patient. Still, it is necessary for fistulas of more than 2 cm in size, after irradiation, after failed repair, if there is a need for simultaneous abdominal surgery (ureteral injury or intestinal fistula), or if a too narrow vagina hinders the vaginal approach.
Surgical technique of the abdominal approach:
- Lower midline laparotomy
- Sagittal incision of the posterior bladder wall into the fistula and excision of the fistula.
- Mobilization of the bladder from the anterior vaginal wall.
- Single-layer closure of the vagina.
- Mobilization of a peritoneal flap or omentum flap to cover the vaginal defect.
- Two-layer closure of the bladder wall (urothelium and tunica muscularis).
- Insert a drain. Transurethral catheter for bladder drainage. Check vesical integrity after two weeks with cystography and remove the catheter.
Palliative Cystectomy for Vesicovaginal Fistula:
Cystectomy is an option in vesicovaginal fistula due to advanced tumor disease or a contracted bladder after radiation therapy.
| Radiation cystitis | Index | Cystitis cystica |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Chapple, C. & Turner-Warwick, R. Vesico-vaginal fistula, BJU Int, 2005, 95, 193-214.
 Deutsche Version: Vesikovaginale Fistel
Deutsche Version: Vesikovaginale Fistel