You are here: Urology Textbook > Bladder > Bladder diverticulum
Bladder Diverticulum: Etiology, Diagnosis and Treatment
Definition
The bladder diverticulum is an outpouching of the bladder wall (Powell et al., 2009). In pseudodiverticula, only the mucous membrane of the bladder herniates; the diverticulum wall is without a muscle layer. In true diverticula, the outpouching consists of all bladder wall layers.
 |
Etiology
Congenital diverticula:
Congenital diverticula are caused by a weakness of the urinary bladder wall, particularly often in the area of the orifice (Hutch diverticulum). They are often associated with vesicoureteral reflux and the ureter may drain into the diverticulum. Diverticula may be caused by abnormalities of the urachus at the bladder dome. Congenital bladder diverticula are sometimes true diverticula with herniation of all wall layers.
Acquired diverticula:
Acquired diverticula are caused by chronically increased pressure during voiding, which leads to the herniation of the bladder mucosa through weak gaps of the muscular layer (pseudodiverticula). A pseudocapsule forms around the diverticulum wall, which is helpful in resecting the diverticulum. The narrow, sphincter-like diverticulum neck increases the urinary stasis in the diverticulum.
- BPH: men over 50
- Neurogenic lower urinary tract dysfunction, especially with detrusor-sphincter-dyssynergia.
- Urethral valves: affects boys.
- Iatrogenic: after insufficient bladder suturing.
Sign and Symptoms
LUTS (also due to the underlying disease), recurrent urinary tract infections, bladder stone formation.
Diagnosis
Urine:
Urine culture and treat possible infection before therapy.
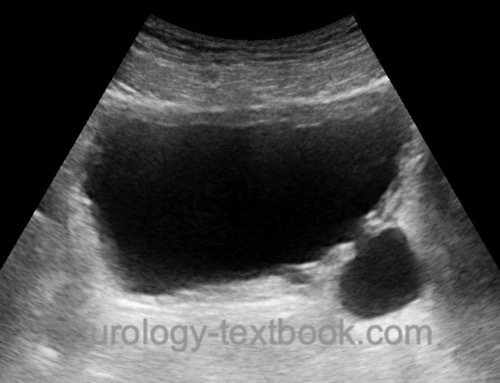
Ultrasound imaging:
Diverticula can be best identified with a full bladder [fig. US imaging of sall bladder diverticulum and US of a large diverticulum]. The kidney is examined to exclude hydronephrosis or to identify a duplex kidney.
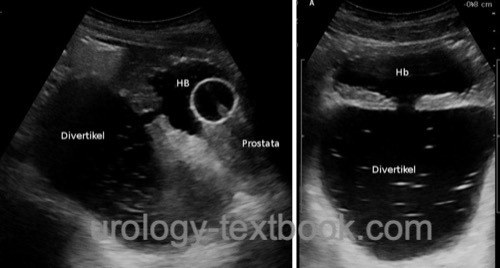 |
VCUG:
Cystography is done with several projections (lateral and a.p.) for exact documentation of size and location [fig. Cystography of a bladder diverticulum]. The residual volume of the diverticulum after voiding is a factor for treatment decisions.
 |
 |
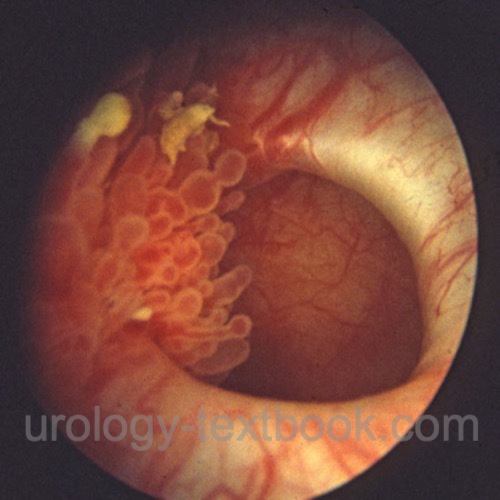
Cystoscopy:
Cystoscopy focuses on the bladder and diverticulum mucosa for suspicious lesions, which should be biopsied (Cave: thin diverticulum wall). Assess the diverticulum size, anatomical relationship between the diverticulum neck and the ureter, and prostatic urethra for subvesical obstruction.
 |
 |
Imaging of the upper urinary tract:
Ultrasound imaging is sufficient; if there are abnormalities, intravenous urography, retrograde pyelography, or CT may be necessary.
Urodynamics:
Urodynamic studies are sometimes necessary for the diagnosis of unclear micturition disorders.
Treatment of Bladder Diverticulum
Conservative therapy:
Significant bladder diverticula with subvesical obstruction of high-risk surgical patients may be managed with permanent catheterization or, if possible, intermittent self-catheterization.
Endoscopic therapy:
Bladder diverticula may be treated endoscopically during subvesical desobstruction: resection of the narrow diverticulum neck to improve communication with the urinary bladder and coagulation of the diverticulum mucosa to induce scarring and shrinkage. Size is the limiting factor for endoscopic therapy, and controlled trials are unavailable (Adachi et al., 1991).
Surgical therapy:
Various surgical techniques for resection of bladder diverticula are possible, see also section bladder diverticulectomy.
- Transvesical diverticulum resection: suitable for the therapy of small bladder diverticula.
- Extravesical diverticulum resection: suitable for treating large bladder diverticula. The technique can be performed with open surgery or laparoscopy, depending on the need for simultaneous desobstruction of the prostate or ureter reimplantation. Inserting a ureteral splint and a transurethral catheter into the diverticulum before surgical therapy simplifies orientation.
| UTI in pregnancy | Index | Bladder stones |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Adachi, M.; Nakada, T.; Yamaguchi, T.; Suzuki, H.;
Hirano, J.; Hirano, K.; Hashimoto, T.; Iijima, Y.; Ishii, N. & Gotoh, Y.
Transurethral
treatment of bladder diverticula.
Eur. Urol. 1991, 19, 104-108.
Powell, C. R. & Kreder, K. J.
Treatment of
bladder diverticula, impaired detrusor contractility, and low bladder
compliance.
Urol Clin North Am 2009, 36, 511-25.
 Deutsche Version: Diagnose und Therapie von Harnblasendivertikel
Deutsche Version: Diagnose und Therapie von Harnblasendivertikel