You are here: Urology Textbook > Surgery (procedures) > Hypospadias surgery
Hypospadias Surgery: Surgical Techniques and Complications
General Principles of Hypospadias Surgery
Timing and Indications
The ideal time for surgery is considered to be the 12th to 18th month of life. Surgery in young children is uncontroversial in marked hypospadias (proximal forms) and hypospadias with relevant urethral stenosis.
Contraindications
- Urinary tract infections
- Coagulation disorders
- Increased surgical risk due to comorbidity
- In distal hypospadias without concomitant pathology, the patient's ability to consent should be awaited (Carmack et al., 2016).
- In intersex patients, hypospadias surgery (as non-vital gender reassignment surgery) is not allowed before puberty without the consent of the family court.
Preoperative Patient Preparations
- Hormone therapy: androgen stimulation is used in patients with micropenis or severe hypospadias. Androgenic therapy results in disproportionate penile growth, which reduces the severity of hypospadias and increases tissue for reconstruction. Hormone therapy is controversial and may lead to subsequent fertility dysfunction. Options include local ointment therapy or parenteral (IM) administration of e.g., testosterone enanthate or HCG.
- Perioperative antibiotic prophylaxis: e.g., with cephalexin until the transurethral catheter is removed. Perioperative antibiotic therapy reduces the rate of bacteriuria, fistulae, meatus stenosis and complicated urinary tract infections.
- Anesthesia: general anesthesia. The penile nerve block before and after surgery facilitates anesthesia management and significantly reduces the child's pain postoperatively.
- Patient positioning: supine position.
Surgical Principles of Hypospadias Repair
- Orthoplasty: penile straightening after artificial erection with plication technique or with grafting in case of short penis or severe curvature.
- Urethroplasty: reconstruction of the missing urethra. The below-mentioned surgical techniques differ mainly in the urethroplasty technique: pedicled flaps, incision of the urethral plate and tubularization, or two-stage surgical techniques.
- Coverage of the neourethra: using a second layer of well-vascularized tissue, mostly raised from the preputium, penile shaft, or scrotal tunica dartos.
- Meatoplasty and glanuloplasty: reconstruction of the meatus and glans to achieve a slit-like meatus.
- Wound closure: after resection or transfer of remaining prepuce.
MAGPI Procedure
MAGPI stands for meatal advancement and glanuloplasty (Duckett et al., 1981a). The technique advances the meatus to the tip of the glans without true lengthening of the urethra.
Indications
Distal (glanular) hypospadias (cosmetic indication). See the section above for general information about indications, timing, contraindications, and patient preparation for hypospadias surgery.
Specific Contraindications:
Significant penile deviation, small glans, and significant (more than glanular) hypospadias.
Surgical Technique:
Place a feeding tube into the bladder and place a traction suture in the glans a the desired position for the new meatus. Continue with a subcoronal circumferential incision and deglove the penile shaft. Advance the dorsal part of the meatus with a deep longitudinal incision from the meatus to the tip of the glans and horizontal closure. Place traction sutures on both wings of the penile glans after blunt mobilization. Advance the ventral part of the meatus with a traction suture. Rotate the glans wings over the ventral part of the urethra and reconstruct the glans with a two-layer closure.
Complications:
Low complication rate: unfavorable cosmetic outcome of the meatus, stenosis, retraction, or fistula (1%). See also the section below for general complications.
Tubularized Incised Plate (TIP) Urethroplasty
TIP urethroplasty is a technique for tubularizing the urethral plate (Snodgrass, 1994). It is a common procedure and is considered technically simple with a low complication rate; the cosmetic result of the glans and the meatus is good.
Indications:
Distal and penile hypospadias. TIP is also recommended by some authors for proximal hypospadias and redo hypospadias surgery with a well-preserved urethral plate. See the section above for general information about indications, timing, contraindications, and patient preparation for hypospadias surgery.
Specific contraindications:
Severe ventral penile curvature forcing resection of the chorda.
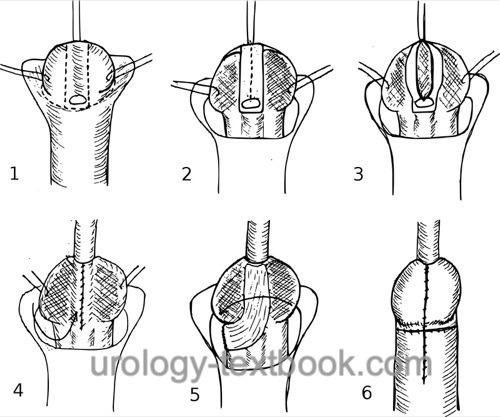 |
Complications:
Urethral stricture (5%) or fistula (4–13%). See also the section below for general complications.
Mathieu Procedure
The Mathieu procedure is a local flip-flap technique for distal hypospadias. A rectangle of skin over the proximal urethra is raised and flipped distally to cover the urethral plate (Mathieu, 1932).
Indications:
Coronal and distal-penile hypospadias without significant ventral curvature, for redo procedures. See the section above for general information about indications, timing, contraindications, and patient preparation for hypospadias surgery.
Specific contraindications:
Unsuitable ventral penile shaft skin proximal to the meatus.
Surgical technique of the Mathieu Hypospadias Repair:
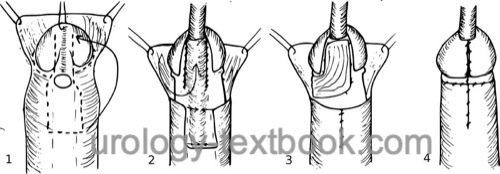 |
Complications:
Transverse rounded meatus, urethral stricture (2%) or fistula (13%). See also the section below for general complications.
Onlay or Tubularized Island Flap
A pedicled preputial flap (=island) is used to reconstruct the missing urethra (Duckett, 1981b). The flap is rotated around the penis and used with an onlay technique to cover the preserved urethral plate. A tubular island flap is possible after resection of the urethral plate.
Indications
Penile hypospadias, with or without resection of the urethral plate. See the section above for general information about indications, timing, contraindications, and patient preparation for hypospadias surgery.
Specific Contraindications:
Missing preputium.
Surgical technique
- Circumferential incision and degloving of the penile shaft, deep incisions between the urethral plate and glans wings.
- Correct penile deviation, if possible without resection of the urethral plate.
- Mobilize a pedicled skin flap (island flap) of inner preputial skin, adjust length and width to cover the urethral plate. The island flap is rotated around the shaft to the urethral plate.
- Without resection of the urethral plate: continuous running suture on both sides of the urethral plate with the rotated island flap.
- After resection of the urethral plate: the island flap is tubularized around the transurethral stent and closed with a continuous running suture. The tubularized island flap is then sutured to the existing urethra.
- Cover the neourethra with a second layer of well-vascularized tissue from the preputium, penile shaft or scrotum.
- Glanuloplasty and wound closure.
Complications:
Urethral diverticula, urethral stricture or fistula, rotation of the penile shaft. See also the section below for general complications.
Two-Stage Hypospadias Repair
Indications:
Proximal hypospadias or redo hypospadias surgery (Johal et al., 2006). See the section above for general information about indications, timing, contraindications, and patient preparation for hypospadias surgery.
Surgical Technique:
- First stage: resect the urethral plate if necessary to correct ventral penile curvature. Cover the tissue defect with a free graft from the prepuce. If resection of the urethral plate is unnecessary, proximal hypospadias can be turned into distal hypospadias by TIP urethroplasty.
- The second stage is done after healing of the graft, which takes several months. Perform a circumferential skin incision around the graft. The lateral edges of the graft are mobilized without compromising the vascular supply. A neo-urethra is formed and closed with a running longitudinal suture. The neourethra is covered with a pedicled Dartos flap from the prepuce or scrotum.
Complications:
Complications are common and often require additional operations (43%): glans dehiscence, fistulas, diverticula, and strictures (Cousin et al., 2022). See also the section below for general complications.
Postoperative Care
Urinary drainage:
Usually a thin dribbling ureteral stent draining into a diaper is used for several days. A suprapubic catheter is a safe alternative if longer urinary drainage is necessary after a complicated repair. Distal uncomplicated hypospadias surgery is possible without urinary drainage.
Postoperative dressings:
Postoperative dressings reduce edema and the risk of postoperative bleeding and are applied for several days to a week (with the dribbling stent). Modern self-adhesive soft foam dressings can be easily removed. A short anesthesia is usually required for the renewal or change of a dressing. After simple hypospadias surgery, an antiseptic ointment dressing is also sufficient. The extent and duration of postoperative dressings are controversial.
Complications After Hypospadias Surgery
Bleeding, hematoma, wound infection, urinary tract infections, flap necrosis, dehiscence of glans correction, meatal or urethral stricture, urethrocutaneous fistula, urethral diverticulum, inadequately corrected penile curvature, chronic LUTS, erectile dysfunction, and impaired ejaculation.
| Two-stage urethroplasty | Index | penile-nerve-block |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Baskin 2000 BASKIN, L. S.:
Hypospadias and urethral development.
In: J Urol
163 (2000), Nr. 3, S. 951–6
A. Carmack, L. Notini, and B. D. Earp, “Should Surgery for Hypospadias Be Performed Before An Age of Consent?,” J Sex Research, vol. 53, no. 8, pp. 1047–1058, 2016.
Cousin et al., “Complication rates of proximal hypospadias: meta-analyses of four surgical repairs.,” J Pediatr Surg., vol. 18, no. 5, pp. 587–597, 2022, doi: 10.1016/j.jpurol.2022.08.005.
DGKCH and DGU, “S2k Leitlinie zur operativenBehandlung der distalen, mittlerenund proximalen Hypospadie.” Accessed: Jan. 05, 2025. [Online]. Available: https://register.awmf.org/assets/guidelines/006-026l_S2k_Operative-Behandlung-distale-mittlere-proximale-Hypospadie_2021-09-verlaengert.pdf
Duckett 1981a DUCKETT, J. W.:
The island flap technique for hypospadias repair.
In: Urol Clin North Am
8 (1981), Nr. 3, S. 503–11
Duckett 1981b DUCKETT, J. W.:
MAGPI (meatoplasty and glanuloplasty): a procedure for subcoronal
hypospadias.
In: Urol Clin North Am
8 (1981), Nr. 3, S. 513–9
EAU guidelines: Paediatric Urology
Mathieu 1932 MATHIEU, P.:
Traitement en un temps de l’hypospadias balanique ou juxtabalanique.
In: J Chir
39 (1932), S. 481?486
Mouriquand u.a. 1995 MOURIQUAND, P. D. ;
PERSAD, R. ; SHARMA, S.:
Hypospadias repair: current principles and procedures.
In: Br J Urol
76 Suppl 3 (1995), S. 9–22
C. Radmayr, G. Bogaert, H. S. Dogan, and Tekgü, “EAU Guidelines: Paediatric Urology,” 2022. [Online]. Available: https://uroweb.org/guidelines/paediatric-urology/.
W. Rodprasert, J. Toppari, and H. E. Virtanen, “Endocrine Disrupting Chemicals and Reproductive Health in Boys and Men.,” Front Endocrinol., vol. 12, p. 706532, 2021.
Snodgrass 1994 SNODGRASS, W.:
Tubularized, incised plate urethroplasty for distal hypospadias.
In: J Urol
151 (1994), Nr. 2, S. 464–5
 Deutsche Version: Technik und Komplikationen von Hypospadie-Operationen
Deutsche Version: Technik und Komplikationen von Hypospadie-Operationen
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.