You are here: Urology Textbook > Surgery (procedures) > Laparoscopic pyeloplasty
Laparoscopic Pyeloplasty: Surgical Steps and Complications
Indications for Pyeloplasty
Pyeloplasty is indicated as surgical therapy for ureteropelvic junction obstruction:
- with scintigraphic evidence of obstruction or
- with decreasing (but sufficient) renal function of the affected kidney or
- with clinical symptoms (flank pain, nephrolithiasis, or recurrent infections)
Pyeloplasty is possible open-surgically and laparoscopically; laparoscopy is recommended for patients without previous perirenal surgery (the majority).
 |
Contraindications for Laparoscopic Pyeloplasty
Nonfunctioning kidney (under 20% of total renal clearance). Coagulation disorders. Comorbidity, which prohibits elective surgery. Consider lumbar open pyeloplasty if the patient had significant previous intraabdominal surgery (like colon or liver surgery) or for re-do pyeloplasty.
Surgical Technique of Laparoscopic Pyeloplasty
Preoperative Patient Preparation
- Exclude or treat urinary tract infection
- Insert a DJ ureteral stent and ensure the diagnosis with retrograde pyelography before surgery.
- Perioperative antibiotic prophylaxis
- Insertion of a transurethral catheter.
- Gastric feeding tube during surgery to empty the stomach.
Surgical Approach via Laparoscopy
Patient Positioning:
The patient is positioned in a lateral position at an angle of 45 degrees and with mild lumbar hyperextension. A vacuum mattress enables a secure patient fixation, even if the operation table has to be tilted.
Trocar positions:
Create a pneumoperitoneum with a mini-laparotomy or the Veress needle next to the umbilicus (camera trocar 10 mm). Insert a second 10 mm trocar slightly caudal to the navel lateral to the ipsilateral rectus. Place a 5 mm trocar between the xiphoid and umbilicus in the midline. Use an additional 5 mm trocar (if necessary) to retract the liver, colon, or spleen, e.g., below the xiphoid or rib cage.
Surgical Approach to the Kidney:
Start with a laterocolic incision to mobilize the colon to the medial. The correct layer between the meso of the colon and retroperitoneum is found most easily below the kidney. After sufficient colon mobilization, identify the ureter at the lower pole of the kidney and continue dissection until the renal pelvis is reached. Watch out for crossing vessels to the lower pole of the kidney. The anterior and posterior aspects of the renal pelvis and the lower pole of the kidney are completely dissected.
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
Pyeloplasty:
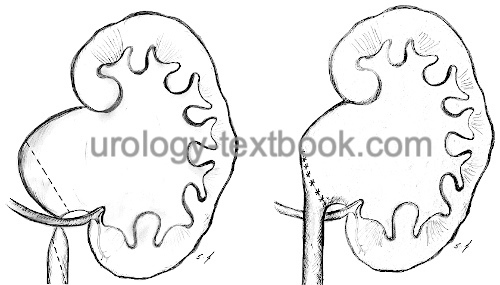
Dismembered pyeloplasty is the method of choice if a crossing vessel is identified as the cause of the UPJ obstruction and probably for most other indications. Place traction sutures at the renal pelvis. The sutures are brought to the outside transcutaneously with the help of a trocar incision closure system and secured with small clamps. The sutures are very helpful for the exposure of the renal pelvis. Excise the UPJ obstruction with, if necessary, excess renal pelvis (reduction pyeloplasty). Spatulate the ureter along the lateral wall (2–3 cm) [fig. laparoscopic dismembered pyeloplasty A to C]. Reposition the ureter concerning the crossing vessels, resulting in an anastomosis ventral of the crossing vessels.
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
Use Vicryl 4-0 as suture material. The anastomosis is done as an interrupted suture. After the first (corner) sutures, the position of the ureteral stent is controlled. Exposure to posterior anastomosis is possible with the help of traction sutures. If in doubt, control the watertightness of the anastomosis by filling the bladder until reflux to the kidney is observed. A drain near the anastomosis is unnecessary in most cases.
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
Drainage:
Drainage of the renal fossa is unnecessary in most cases.
Technical modifications:
The following modifications of laparoscopic pyeloplasty may be used in combination:
- Retroperitoneoscopic pyeloplasty: is technically more challenging, but reduces postoperative pain and hospital stay (Singh et al., 2014).
- Robot-assisted laparoscopy: the three-dimensional view, articulated instruments with several degrees of freedom, a filtered hand tremor and the ergonomic working position simplify laparoscopic surgery. Since pyeloplasty is a demanding procedure concerning the laparoscopic expertise, the use of the robot is justified to avoid open surgery.
- Single-port laparoscopy: the surgery is performed via a trocar with multiple channels and with special angulated instruments. There is also a single-port platform available for robot-assisted laparoscopy (Dobbs et al., 2020).
Care after Pyeloplasty
General Measures:
Early mobilization. Respiratory therapy. Thrombosis prophylaxis. Laboratory controls (Hb). Wound inspections.
Analgesia:
Analgesics with a combination of NSAIDs and opioids.
Drains and Catheters:
Remove the drainage if the daily drainage volume is below 50 ml. Leave the foley catheter for an additional 1–2 days (or 3–5 days without drainage), and the ureteral stent for 2–4 weeks.
Complications of Pyeloplasty
In principle, the same complications are possible as with open pyeloplasty. The laparoscopic technique reduces approach-related complications. The success rate of renal pyeloplasty (sufficient urine drainage in the long term) is high, at over 95% for primary surgery patients. The success rate for recurrent surgery is significantly lower at 84% (Inagaki et al., 2005).
- Insufficiency of the anastomosis: urinoma, urinary peritonitis, recurrent ureteral stricture, loss of renal function.
- General surgical risks: Bleeding, wound infection, urinary tract infection, injury to neighboring organs (liver, spleen, intestine and pancreas). Incisional hernia (due to subcostal nerve injury).
| Open pyeloplasty | Index | Ureteroureterostomy |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
P. Bove, A. M. Ong, K. H. Rha, P. Pinto, T. W. Jarrett, and L. R. Kavoussi, “Laparoscopic management of ureteropelvic junction obstruction in patients with upper urinary tract anomalies,” J Urol, vol. 171, no. 1, pp. 77–9, 2004.
Inagaki T, Rha KH, Ong AM, Kavoussi LR, Jarrett TW. Laparoscopic pyeloplasty: current status. BJU Int. 2005 Mar;95 Suppl 2:102-5. doi: 10.1111/j.1464-410X.2005.05208.x.
Singh V, Sinha RJ, Gupta DK, Kumar V, Pandey M, Akhtar A. Prospective randomized comparison between transperitoneal laparoscopic pyeloplasty and retroperitoneoscopic pyeloplasty for primary ureteropelvic junction obstruction. JSLS. 2014 Jul-Sep;18(3):e2014.00366. doi: 10.4293/JSLS.2014.00366.
J. A. Smith, S. S. Howards, G. M. Preminger, and R. R. Dmochowski, Hinman’s Atlas of Urologic Surgery Revised Reprint. Elsevier, 2019.
C. Radmayr, G. Bogaert, H. S. Dogan, and S. Tekgül, “EAU Guidelines: Paediatric Urology.” [Online]. Available: https://uroweb.org/guidelines/paediatric-urology/
B. J. Tan and A. D. Smith, “Ureteropelvic junction obstruction repair: when, how, what?,” Curr Opin Urol, vol. 14, no. 2, pp. 55–9, 2004.
 Deutsche Version: Laparoskopische Nierenbeckenplastik
Deutsche Version: Laparoskopische Nierenbeckenplastik
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.