You are here: Urology Textbook > Examinations > Voiding Cystourethrography (VCUG)
Technique of Voiding Cystourethrography (VCUG) and Normal Findings
Indications
The examination can be performed as a simple cystography (without voiding) or as a voiding cystourethrography [fig. VCUG] depending on the clinical question:
Static cystography:
Trauma to the bladder, bladder stones, bladder diverticulum, bladder fistula, after surgery of the bladder or prostate.
Voiding cystourethrography:
Vesicoureteral reflux, urinary incontinence, pelvic floor insufficiency, neurogenic lower urinary tract dysfunction.
 |
Examination Technique of Voiding Cystourethrography (VCUG)
Voiding cystourethrography:
It is necessary to insert a transurethral catheter for the examination; this can be used as a post-void residual urine test if needed. The bladder is slowly filled with body warm contrast medium, while the patient reports the filling state of the bladder. If there is a strong urge to urinate, the filling of the bladder is stopped and the volume correlates with the functional bladder capacity.
X-ray images of the urinary bladder are done in two projections (a.p. and lateral or oblique films). In examinations for stress incontinence and pelvic floor insufficiency, films with and without the Valsalva maneuver in lateral projection are obtained [fig. VCUG in stress urinary incontinence]. The vagina and the urethra are marked with contrast medium or a small metal chain for orientation [fig. VCUG in cystocele]. After removal of the indwelling catheter, the patient urinates under fluoroscopy to assess the urethra [fig. normal voiding cystourethrography].
 |
 |
Cystography
The examination is limited to filling the bladder with contrast medium via a transurethral catheter (see above). X-ray images of the urinary bladder are done in two projections (a.p. and lateral or oblique films); further images are obtained after emptying the bladder via the catheter to look for contrast medium extravasations.
Normal Findings of Voiding Cystourethrography (VCUG)
Capacity of the bladder:
Women 250–550 ml, men 350–750 ml. The bladder capacity in children is estimated using the following formula:
Capacity in ml = (Age in years + 2) × 30
Differential diagnosis of low bladder capacity:
Incontinence, bladder wall inflammation, fibrosis, radiation, surgery, bladder carcinoma, extravesical tumor, neurogenic bladder, overactive bladder. Diseases of the bladder wall lead to passive low bladder capacity, which leads to a constant pressure increase during bladder filling. In active low bladder capacity, neurological factors lead to an inconstant reduced bladder capacity with autonomic detrusor contractions.
Differential diagnosis of high bladder capacity:
Damage to the afferent bladder nerves (diabetes, syphilis), atonic bladder paralysis, overdistention in (chronic) subvesical obstruction, congenital megacystis, chronic infections.
 |
Cystography:
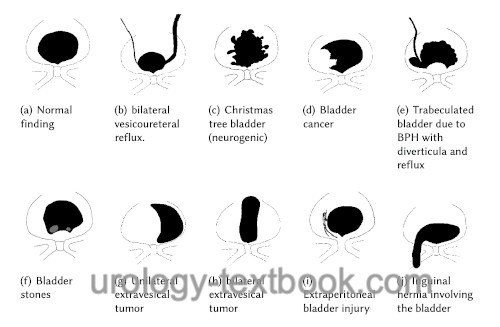
The bladder wall is smooth without diverticulum or filling defects. Please see fig. differential diagnosis of cystography for schematic drawings of common findings. The micturition is initiated with the opening of the inner bladder neck; this can be seen in the lateral projection. There should not be any vesicoureteral reflux during the passive filling or active emptying of the bladder. Residual urine, if any, should be under 10% of the bladder capacity.
Sensibility of the bladder:
The functional bladder capacity measured with VCUG is lower than in micturition diaries. Overdistention during the examination should be avoided; it weakens the detrusor activity.
| Intravenous urography | Index | Retrograde Urethrography |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
 Deutsche Version: Miktionszysturethrographie (MCU)
Deutsche Version: Miktionszysturethrographie (MCU)