You are here: Urology Textbook > Surgery (procedures) > Urinary diversion
Ileal Conduit: Surgical Technique (Step-by-Step) and Complications
Definition and Indications for Ileal Conduit
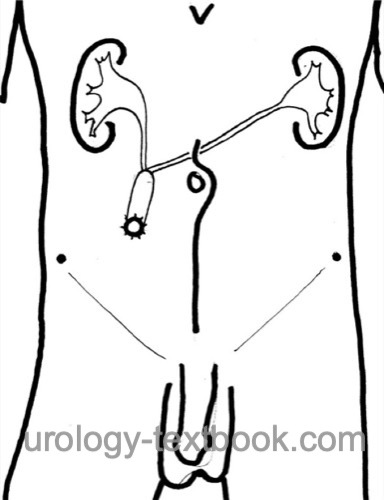
The ileal conduit is an incontinent heterotopic urinary diversion after cystectomy [fig. ileal conduit]. The ureters are anastomosed with a short ileal loop, which is passed through the abdominal wall as a stoma.
In patients with contraindications to continent urinary diversion (see previous section urinary diversion), the ileal conduit is the most commonly used urinary diversion. Advantages include simple technique, short bowel requirement, low long-term metabolic complications, and avoidance of transurethral incontinence. The disadvantage is the need for stoma care.
 |
Contraindications for Ileal Conduit
- Diseases of the small bowel: irradiation, short bowel syndrome, Crohn disease. Consider a colon conduit as an alternative.
- Multimorbid patients with a short life expectancy: consider ureterocutaneostomy.
Step-by-Step Surgical Technique of Ileal Conduit
Preoperative patient preparation:
Please see the section on radical cystectomy.
Ileal Dissection:
Choose a distal ileum loop of 20 cm length and at least 20 cm distance from the ileocecal valve; see the section bowel anastomosis for the surgical technique. Antiseptic irrigation of the isolated bowel loop. End-to-end anastomosis of the remaining bowel (ileoileostomy).
Dissection of the ureters:
The ureters are splinted with MJ ureteral stents (secured with 4-0 fast absorbing sutures), which allows for the atraumatic management of the ureters during the next steps. Dissect the ureters as little as possible to maintain their blood supply (caution: ureteral stricture). Create a tunnel crossing the great vessels under the mesentery of the colon and bowel from the left to the right retroperitoneum with blunt finger dissection. Bring the left ureter to the right lower abdomen using the tunnel.
Uretero-ileal anastomosis (Bricker technique):
Close the oral end of the ileal loop with a running suture (PDS 4-0). The ureters are spatulated and anastomosed separately at the antimesenteric side of the conduit (interrupted sutures PDS 4-0). The ureteral stents are passed through the ileal segment before anastomosis.
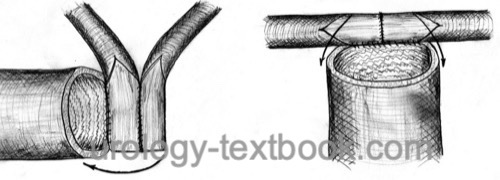 |
Uretero-ileal anastomosis (Wallace technique):
The ureters are widely spatulated and conjoined (side-to-side anastomosis with PDS 4-0). The ureteral plate is anastomosed to the ileal segment with a running suture [fig. uretero-ileal anastomosis]. The ureteral stents are passed through the ileal segment before anastomosis.
Stoma:
The location of the stoma should be 5 cm from the wound incision and pass through the rectus abdominis muscle. The ideal location is an infraumbilical fat roll over the right rectus abdominis muscle. Mark the stoma location on the sitting patient before surgery. Create a circular skin incision (1.5 cm in diameter). Split the fascia crosswise, dissect the rectus bluntly, and incise the peritoneum. Two fingers should fit comfortably through the opening.
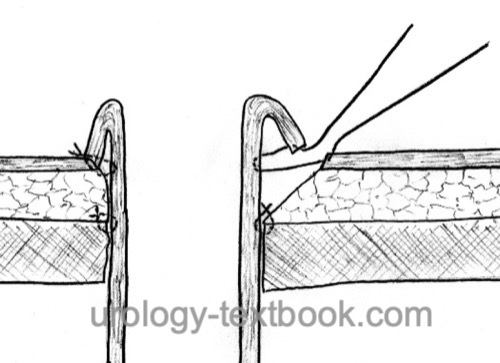 |
Pass the aboral end of the ileal conduit through the opening; the length should extend approximately 5 cm above the skin level. Secure the conduit to the fascia (8 interrupted sutures with PDS 2-0). Suture the ileal end to the dermis and create a prominent nipple-shaped stoma [fig. \ref{ileum-conduit-stoma}]. In obese patients, a loop-end ileostomy is an excellent technical alternative.
Postoperative Care after Ileal Conduit
Please see the section urinary diversion for postoperative care.
Complications of Ileal Conduit
In addition to the complications of radical cystectomy, significant complications are possible, some occurring years after surgery (Shimko et al., 2011):
- Complications of bowel anastomosis (10–20%): obstruction, ileus, fistula or abscess.
- Ischemia and necrosis of the ileal conduit (rare)
- Complications of uretero-ileal anastomosis: urine leakage with urinoma, strictures with hydronephrosis (10%)
- Urinary tract infections, urosepsis
- Urinary stone formation (15%)
- Stoma complications in 15%: dermatitis, stoma stenosis, stomal retraction, or hernia.
| Radical cystectomy | Index | Ileal conduit |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Hautmann 2003 HAUTMANN, R. E.:
Urinary diversion: ileal conduit to neobladder.
In: J Urol
169 (2003), Nr. 3, S. 834–42
Shimko MS, Tollefson MK, Umbreit EC, Farmer SA, Blute ML, Frank I. Long-term complications of conduit urinary diversion. J Urol. 2011 Feb;185(2):562-7. doi: 10.1016/j.juro.2010.09.096.
 Deutsche Version: Technik und Komplikationen des Ileumkonduits
Deutsche Version: Technik und Komplikationen des Ileumkonduits
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.