You are here: Urology Textbook > Surgery (procedures) > Ureterocutaneostomy
Ureterocutaneostomy: Surgical Technique (Step-by-Step) and Complications
Definition and Indications for Ureterocutaneostomy
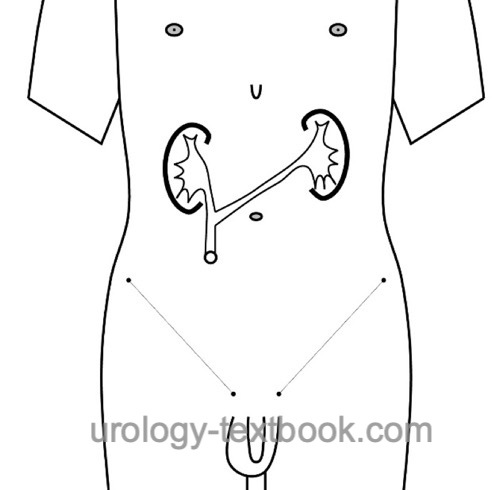
Ureterocutaneostomy is a simple heterotopic incontinent urinary diversion that can be constructed without using the bowel [fig. ureterocutaneostomy and RPG of ureterocutaneostomy]. The decisive disadvantage of ureterocutaneostomy is the frequent need for permanent ureteral splinting.
In the following situations, ureterocutaneostomy should be preferred to a conduit: short life expectancy, high comorbidity, need to avoid a bowel anastomosis, e.g., after radiotherapy, multiple abdominal procedures, or in patients with short bowel syndrome.
 |
 |
Step-by-Step Surgical Techniques of Ureterocutaneostomy
Preoperative patient preparation:
Please see the section on radical cystectomy.
Ureteral dissection:
Create a tunnel crossing the great vessels under the mesentery of the colon and bowel from the left to the right retroperitoneum with blunt finger dissection. Bring the shorter ureter to the contralateral lower abdomen using the tunnel. The shorter ureter is anastomosed end-to-side to the longer ureter. First, incise the longer ureter over 3 cm medially and longitudinally in the area of the planned anastomosis. Spatulate the shorter ureter distally over 3 cm. Place corner sutures (PDS 4-0) for the anastomosis and splint both ureters with MJ ureteral stents. Suture the posterior wall of the anastomosis in a running fashion from the inside and the anterior wall of the anastomosis from the outside (see also section transureteroureterostomy).
Stoma:
Spatulate the distal end of the longer ureter [fig. ureterocutaneostomy stoma]. Perform a circular skin incision at the previously marked stoma location (1.5 cm in diameter). Split the fascia crosswise, dissect the rectus bluntly, and incise the peritoneum. One finger should fit comfortably through the opening. Bring the distal end of the longer ureter through the channel and suture the end to the cutis. Secure the ureteral splints with sutures.
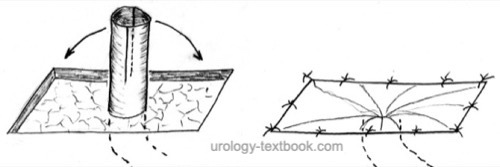 |
Omentum flap:
A omentum flap can help to protect the passage of the ureter through the abdominal wall, prevent stoma stenosis and permanent ureteral splinting. A sufficiently long and 5 cm wide omentum flap is wrapped around the ureters and fixed separately to the skin, rectus sheath, and peritoneum. The spatulated end of the ureter is now attached to the omentum flap instead of to the skin (Lodde et al., 2005).
Postoperative Care after Ureterocutaneostomy
Please see the section urinary diversion for postoperative care.
Complications of Ureterocutaneostomy
In addition to complications of cystectomy: dislocation of ureteral stents, hydronephrosis, urinary tract infections and urinary stone formation, and stoma complications (dermatitis, stoma stenosis, stomal retraction or hernia).
| Colon conduit | Index | Ileal neobladder |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Hautmann 2003 HAUTMANN, R. E.:
Urinary diversion: ileal conduit to neobladder.
In: J Urol
169 (2003), Nr. 3, S. 834–42
Shimko MS, Tollefson MK, Umbreit EC, Farmer SA, Blute ML, Frank I. Long-term complications of conduit urinary diversion. J Urol. 2011 Feb;185(2):562-7. doi: 10.1016/j.juro.2010.09.096.
 Deutsche Version: Technik und Komplikationen des Kolonkonduits
Deutsche Version: Technik und Komplikationen des Kolonkonduits